Introduction
Among the lesions of the spine, accompanied by neurological manifestations, the most common are degenerative-dystrophic processes. They are among the most common pathologies, and the rate of neurological manifestations of degenerative-dystrophic lesions of the spine in all diseases of the peripheral nervous system is significant [1].
Seronegative spondyloarthropathy (SpA) is a group of interrelated clinically intersecting chronic inflammatory rheumatic diseases, including idiopathic ankylosing spondylitis (the most typical form), reactive arthritis, psoriatic arthritis and enteropathic arthritis associated with an inflammatory bowel disease. The most characteristic clinical feature of SpA is back pain, which has an inflammatory nature. Differential diagnosis among these forms, especially in the early stages, is not always possible due to the unclear clinical features of different forms, but this usually does not affect the tactics of their treatment [2].
According to current guidelines, patients are prescribed nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and improve quality of life in cases of musculoskeletal disorders. During treatment with this group of drugs, the occurrence of side effects is very common. The main negative property of all NSAIDs is the high risk of side effects from the digestive tract. Dyspeptic disorders are observed in 30–40 % of patients receiving NSAIDs, erosions and ulcers in the stomach and duodenum in 10–20 %, and bleeding and perforations in 2–5 %. Dyspepsia is the main reason for discontinuation of NSAID treatment in more than 50 % of cases. Dyspepsia is most often observed in patients with a history of gastrointestinal pathology [3].
The prevalence of gastroesophageal reflux disease (GERD) in Western populations over the past 30 years has a clear tendency to increase and varies from 10 to 30 % [4, 5]. The study of GERD is also relevant due to both typical and atypical (bronchopulmonary, cardiac, dental, otolaryngological) clinical manifestations of the disease, which complicate the diagnosis of GERD [6]. In the pathogenesis of GERD, as in other acid-dependent pathological conditions, the leading is a disturbance of the balance between aggressive and protective factors in the esophageal mucosa with the predominance of the former [5].
Thus, the study of clinical features, factors and levels of various biologically active substances that may play an important role in the pathogenetic mechanism of GERD in combination with degenerative-dystrophic or inflammatory lesions of the spine, is an extremely important problem of the modern medical community.
The purpose of the study is to determine the peculiarities of changes in the level of serum somatostatin (SST) and its relationship with calcium metabolism in patients with GERD and spine lesions of degenerative-dystrophic and inflammatory genesis.
Materials and methods
84 patients with spinal lesions of degenerative-dystrophic or inflammatory genesis in combination with GERD were examined. The examined patients were hospitalized in Rheumatology, Neurology, Traumatology and Gastroenterology Departments of Municipal Non Profit Enterprise “Transcarpathian Regional Clinical Hospital named аfter Andrii Novak”of Transcarpathian Regional Council, and patients who were on outpatient observation by family doctors at the place of residence, as well as underwent dental treatment at Dental Plus Clinic in the period of 2019–2021. The examined patients with GERD were divided into two groups depending on the form of spine injury. Group I included 44 patients with osteochondrosis of the cervical and thoracic spine, among them there were 26 males (59.1 %) and 18 females (40.9 %), with the average age of (43.7 ± 3.8) years. Group II consisted of 40 patients with spinal arthritis. Among them there were 16 males (40.0 %) and 24 females (60.0 %), with the average age of (46.9 ± 5.1) years.
The control group included 20 healthy individuals: 11 males (55.0 %) and 9 females (45.0 %) without lesions of the musculoskeletal system and upper gastrointestinal tract. The average age was (43.2 ± 4.6) years.
All studies were performed with the consent of patients, and their methodology was in line with the Helsinki Declaration of Human Rights of 1975 and its revision in 1983, the Council of Europe Convention on Human Rights and Biomedicine, and the legislation of Ukraine.
The diagnosis of GERD was established according to the criteria of the unified clinical protocol (order of the Ministry of Health of Ukraine dated 31.10.2013 № 943) taking into account complaints, endoscopic examination data, etc. To confirm the diagnosis, the examined patients underwent fibroesophagogastroduodenoscopy (FEGDS) using endoscopy equipment Pentax ERM-3300 video processor and flexible fiber endoscopes Pentax E-2430, GIF-K20. Also, 24-hour pH monitoring according to the method of Prof. V.N. Chernobrovy was performed. The Los Angeles (LA) classification (1998) was used for endoscopic assessment of the degree of damage to the esophagus: Grade A — one (or more) mucosal break no longer than 5 mm, that does not extend between the tops of two mucosal folds; Grade B — one (or more) mucosal break more than 5 mm long that does not extend between the tops of two mucosal folds; Grade C — one (or more) mucosal break that is continuous between the tops of two or more mucosal folds but which involves less than 75 % of the circumference; Grade D — one (or more) mucosal break which involves at least 75 % of the oesophageal circumference [7].
The diagnosis of spondyloarthritis (SpA) was established on the basis of diagnostic criteria of the American College of Rheumatology (ACR, 2018) and European League Against Rheumatism (EULAR, 2018). Osteochondrosis (OC) of the cervical and thoracic spine was diagnosed on the basis of physical and general clinical me–thods, as well as the results of computed tomography of the above sections of the spine. To study the motor ability of the spine, a functional assessment of spine mobility and muscle strength of the back and abdomen was performed (Schober test, spine extension, finger-floor test, functional tests to determine the strength endurance of the extensor muscles of the back and abdomen), in accordance with the recommendations of the American Academy of Orthopedic Surgeons (AAOS, 2018) [8, 9].
All patients were tested for serum somatostatin level by enzyme-linked immunosorbent assay (ELISA) using Human Somatostatin EIA-1 Kit test system No. 1.03930004301 from Ray Biotech. The level of total calcium (Ca++) in the serum of the examined patients was determined by colorimetric method. The level of 25-hydroxyvitamin D (25(OH)D) was also determined to assess the status of vitamin D in the examined patients using an immunochemical method with electrochemiluminescent detection (ECLIA — Cobas 6000), using Roche Diagnostics (Switzerland) test systems. The level < 20 ng/ml was evaluated as vitamin D deficiency; 20.0 — < 30 ng/ml — insufficiency, and the level ≥ 30 ng/ml was considered optimal. The level of total calcium in the serum was determined by chlorimetric method.
The inclusion criteria were as follows: the presence of clinical symptoms (typical and atypical) of GERD, detection of FEGDS changes in the esophageal mucosa characteristic of GERD, spondyloarthritis, and osteochondrosis of cervical and thoracic spine.
The exclusion criteria were as follows: functional or organic diseases of the esophagus, stomach and duodenum, non-erosive form of GERD, Barrett’s esophagus, Helicobacter pylori positive patients, and patients with psychiatric and oncological diseases.
The analysis and processing of the results of the examinations was performed by the computer program Statistics for Windows v. 10.0 (StatSoft Inc, USA) using parametric and non-parametric methods for evaluating the results.
Results
Complaints of digestive organs characteristic of GERD (typical esophageal manifestations) were more often found in patients of group I — 54.5 % of the examined patients (p < 0.05), while patients of group II were more often diagnosed with extraesophageal forms of GERD — 57.5 % of the examined patients (p < 0.05). The leading clinical manifestation of the upper digestive tract lesions in patients of both groups was acid regurgitation, heartburn, sore throat and dysphagia.
Atypical manifestation of GERD in patients of both groups were more often manifested by dental, otolaryngological “masks”. At the same time, there was a difference: patients of group I with OC of the cervical and thoracic spine more often had dental form of GERD (40.0 % of subjects, respectively — p < 0.05), while patients with SpA were more often diagnosed with otolaryngological “mask” of GERD (43.5 % of examined patients — p < 0.05). The cardiac form of GERD was 7.4 % more common in SpA (p < 0.05), while the bronchopulmonary form of reflux disease was found with almost equal frequency in patients of both groups (15.0 % and 13.0 % of the examined patients, respectively). The results are shown in Table 1.
FEGDS confirmed the diagnosis of GERD in all examined patients in both groups with spinal cord injury of degenerative-dystrophic or inflammatory origin. At endoscopic examination in all patients of both groups it was manifested by gastroesophageal reflux and reflux esophagitis (RE) of varying severity (Table 2)
It was noted that in the group of patients with OS, the severity of RE more often corresponded to LA-B, both in the typical and atypical course of GERD. In patients of group I LA-A and LA-C was found almost with the same frequency (20.8 % and 29.2 % of patients), while none of the patients with typical manifestation of GERD were diagnosed with LA-A. In patients with OS of the spine and atypical manifestation of GERD most often LA-B was detected during FEGDS.
During endoscopic examination, patients of group II with SpA and the typical manifestation of GERD were more often diagnosed with esophageal lesions of LA-B (47.1 % of patients), while in extraesophageal forms of GERD lesions of the esophagus more often corresponded to LA-C. In contrast to patients of group I, with SpA often had candida esophagitis (CE), mainly in the atypical course of GERD. Thus, 40.0 % of patients had dental manifestations and 33.3 % of patients otolaryngological “masks” (p < 0.01).
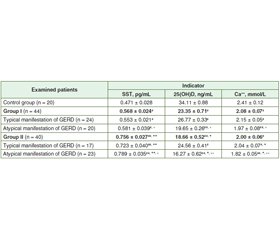
There was a significant increase in the level of serum SST in both groups of the studied patients with GERD and spine injury of degenerative-dystrophic or inflammatory origin. At the same time, a more pronounced deviation from the norm was detected in group II of patients (increase up to (0.756 ± 0.027) pg/ml, p < 0.01). Noteworthy is the change in the level of SST in the serum in both groups of the examined patients depending on the clinical form of GERD, with the maximum increase in patients with atypical manifestation of GERD. Determination of level 25(OH)D in serum indicates vitamin D3 deficiency in patients with GERD and OS (decrease to (23.35 ± 0.71) ng/ml, p < 0.05) and its deficiency in patients with SpA (decrease to (18.66 ± 0.52) ng/ml, p < 0.01). Serum 25(OH)D levels also decreased more markedly in the atypical clinical course of GERD in the examined patients. The analysis of the obtained data indicates a decrease in serum calcium with the maximum deviation from the norm in patients of group II with atypical manifestation of GERD (decrease to (1.82 ± 0.05) mmol/l at a rate of (2.41 ± 0.12) mmol/l, p < 0.01).
Correlation analysis established the relationship between serum SST and a decrease in serum 25(OH)D and Ca++. At the same time, a strong correlation was found between these indicators in patients of group II with the atypical clinical course of GERD; a moderate correlation was found in esophageal manifestations of reflux disease. In patients of group I, the correlation between these indicators was established mainly in patients with atypical manifestation of GERD (Table 5).
Thus, in patients with degenerative-dystrophic and inflammatory lesions of the spine GERD is more often manifested by atypical clinical symptoms. Examination of serum SST level indicates its increase with the most pronounced deviation from the norm in extraesophageal manifestations of GERD. In this case, a correlation was found between the increase in serum SST level and the decrease in the level of 25(OH)D and Ca++ in these patients.
Discussion
Studies of pathogenetic links of GERD formation in various pathological states are being carried out. Especially relevant is the study of the combined course of GERD with diseases that require treatment with NSAIDs, which can adversely affect the condition of the mucous membrane of the upper digestive tract. In this case, exogenous and endogenous factors affect the tonus of the lower esophageal sphincter (LES), contributing to the formation of GERD. It is known that the pressure in the LES decreases under the influence of some hormones of the gastrointestinal tract: glucagon, gastrin, somatostatin, cholecystokinin, secretin, vasointestinal peptide and enkephalin [10]. Thus, several peptide hormones that regulate food consumption (ghrelin, adipokines), gastric acid secretion and gastrointestinal motility play an important role in the formation of GERD. The pathogenesis of GERD is multifactorial, but not completely clear, especially in comorbid conditions [11].
Somatostatin was first identified in extracts of the hypothalamus as a factor capable of inhibiting the release of growth hormone. Subsequent studies have found that SST is widely produced in the body, including other parts of the brain, small intestine, pancreatic islets and stomach. Currently, SST is considered both a hormone and a paracrine regulator. It usually acts as an inhibitor of certain physiological processes, such as gastrin secretion in the stomach and insulin secretion in pancreatic islets. The main amount of circulating SST comes from the intestines, not from pancreatic islets [12].
In our opinion, the study of serum SST that inhibits the level of somatotropic hormone, thus affecting the growth of the body as a whole, in particular calcium metabolism, and possibly LES, can play a significant role in the formation of combined pathology, such as GERD in patients with degenerative-dystrophic and inflammatory lesions of the spine.
Somatostatin plays an important role in regulating metabolic processes, including mineral metabolism [13, 14]. The results of our studies indicate a high level of SST in patients with GERD in combination with OS or SpA of the spine. At the same time, a correlation was found between the decrease in the level of vitamin D3 and calcium and SST in the serum. The high share of atypical forms of GERD in the examined patients with combined pathology is noteworthy. Atypical manifestation of GERD (especially dental and otolaryngological “masks”) of reflux disease are associated with pronounced endoscopic changes, which corresponds to LA-B and LA-C. Thus, in patients with degenerative-dystrophic and inflammatory lesions of the spine, often the signs of GERD can be underestimated by related specialists. In the treatment of these patients a comprehensive approach of doctors of different specialties (dentists, otolaryngologists, pulmonologists, cardiologists, etc.) is required.
Further research in this area is needed to clarify the processes underlying the occurrence/progression of lesions of the digestive organs (especially the upper digestive tract) in patients with degenerative-dystrophic and inflammatory lesions of the spine. Digestive tract lesions should also be considered through the prism of possible adverse effects on musculoskeletal disorders. This is especially evident in dental “masks” of GERD, when the negative impact of acid refluxant causes caries and other changes in the oral cavity, and can also lead to complications during dental implantation.
Conclusions
In patients with GERD with degenerative-dystrophic and inflammatory lesions of the spine, an increase in the level of serum SST was found with the most pronounced deviation from the norm in atypical manifestation of GERD. A correlation between SST and a decrease in the level of 25(OH)D and Ca++, mainly in patients with atypical clinical course of GERD, was established.
Received 11.01.2022
Revised 22.01.2022
Accepted 24.01.2022

/15.jpg)
/16.jpg)