Журнал «Здоровье ребенка» Том 20, №4, 2025
Вернуться к номеру
Збройні конфлікти як чинник ризику розвитку карієсу в дітей
Авторы: O.V. Sheshukova, A.S. Mosiienko, T.V. Polishchuk, N.M. Lokhmatova, S.S. Bauman, V.H. Kostenko, Yu.V. Popelo
Poltava State Medical University, Poltava, Ukraine
Рубрики: Педиатрия/Неонатология
Разделы: Клинические исследования
Версия для печати
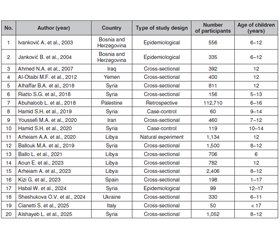
Актуальність. Збройні конфлікти, що охоплюють численні регіони світу, мають деструктивний вплив на всі аспекти життя населення, зокрема здоров’я дітей. Одним із найменш вивчених, але важливих наслідків є погіршення стоматологічного здоров’я в дитячій популяції, що обумовлене комплексом фізіологічних, соціальних та психологічних факторів. Мета: систематичний аналіз впливу збройних конфліктів на поширеність карієсу в дітей і підлітків, визначення основних факторів ризику та пошук ефективних стратегій профілактики й підтримки здоров’я порожнини рота в умовах війни. Матеріали та методи. У березні 2025 року здійснено пошук літератури в базах даних PubMed, Scopus, Web of Science та Google Scholar відповідно до критеріїв PRISMA 2020. Включено лише англомовні публікації до березня 2025 року. Відібрано 20 релевантних досліджень, які охоплюють понад 125 тис. дітей. Результати. Установлено, що основними детермінантами погіршення стоматологічного здоров’я в умовах війни є психоемоційний стрес, посттравматичний стресовий розлад, недоїдання, соціально-економічні труднощі, погана гігієна та відсутність доступу до стоматологічної допомоги. У дітей, які пережили травматичний досвід, відзначаються значно гірші показники карієсу, стану ясен та гігієнічної поведінки. Встановлено прямий зв’язок між поширеністю карієсу й такими факторами, як бідність, освіта батьків, тип проживання. Підтверджено, що обмеження доступу до цукру в окремих випадках знижує захворюваність, проте загальний вплив війни на стоматологічне здоров’я є негативним. Висновки. Необхідне впровадження цільових профілактичних стратегій, зокрема мобільних клінік, телемедицини, гігієнічної освіти, психосоціальної підтримки й волонтерських ініціатив, для забезпечення стоматологічної допомоги дітям у кризових умовах.
Background. Armed conflicts in many regions of the world have a profoundly destructive impact on all aspects of life, including the health of children. One of the least studied yet critically important consequences is the deterioration of children’s oral health, driven by a complex interplay of physiological, social, and psychological factors. The purpose was to conduct a systematic analysis of the impact of armed conflicts on the prevalence of dental caries in children and adolescents, to identify key risk factors and to propose effective strategies for the prevention and maintenance of oral health in wartime conditions. Materials and methods. A literature search was conducted in March 2025 using the PubMed, Scopus, Web of Science, and Google Scholar databases, following the PRISMA 2020 guidelines. Only publications written in English and issued prior to March 2025 were included. A total of 20 relevant studies were selected, encompassing data on more than 125,000 children. Results. The analysis revealed that the primary determinants of deteriorating dental health in war conditions include psycho-emotional stress, post-traumatic stress disorder, malnutrition, socioeconomic hardship, poor oral hygiene, and limited access to dental care. Children exposed to traumatic experiences demonstrated significantly higher rates of dental caries, periodontal disease, and poorer hygiene practices. A direct association has been identified between caries prevalence and factors, such as poverty, parental education level, and type of residence. While some evidence suggests that reduced sugar access during wartime may lower caries incidence in isolated cases, the overall impact of armed conflict on children’s oral health is strongly negative. Conclusions. There is a pressing need for the implementation of targeted preventive strategies, including the deployment of mobile dental clinics, the use of telemedicine, oral hygiene education programs, psychosocial support, and volunteer-based initiatives, to ensure the delivery of essential dental care to children living in crisis settings.
карієс; війна; огляд; діти; демінералізація емалі
dental caries; armed conflicts; review; children; enamel demineralization
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Our World in Data. Number of armed conflicts, World. Oxford: Our World in Data. Available from: https://ourworldindata.org/grapher/number-of-armed-conflicts.
- United Nations High Commissioner for Refugees (UNHCR). Global Trends report 2023. Geneva: UNHCR. Available from: https://www.unhcr.org/global-trends-report-2023.
- Kisely S. No mental health without oral health. Can J Psychiatry. 2016;61(5):277-282. doi: 10.1177/0706743716632523.
- Bourgeois DM, Llodra JC. Global burden of dental condition among children in nine countries participating in an international oral health promotion programme, 2012–2013. Int Dent J. 2014;64(Suppl 2): 27-34. doi: 10.1111/idj.12129.
- Kazeminia M, Abdi A, Shohaimi S, Jalali R, Vaisi-Raygani A, Salari N, Mohammadi M. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: a systematic review and meta-ana–lysis. Head Face Med. 2020;16(1):22. doi: 10.1186/s13005-020-00237-z.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
- Folayan MO, Schroth RJ, Ayouni I, et al. A scoping review lin–king early childhood caries to violence, neglect, internally displaced, migrant and refugee status. BMC Oral Health. 2023;23:747. doi: 10.1186/s12903-023-03459-0.
- Bendavid E, Boerma T, Akseer N, Langer A, Malembaka EB, Okiro EA, et al.; BRANCH Consortium Steering Committee. The effects of armed conflict on the health of women and children. Lancet. 2021;397(10273):522-532. doi: 10.1016/S0140-6736(21)00131-8.
- Kaskova LF, Yanko NV, Sadovski MO, Pavlenkova OS, Vashenko IY, Novikova SCh, Ulasevych LP. Assessment of attitudes and practices regarding oral healthcare among the parents during the war. J Int Dent Med Res. 2024;17(1):203-208.
- Santa Barbara J. Impact of war on children and imperative to end war. Croat Med J. 2006;47(6):891-894.
- Faustova MO, Ananieva MM, Basarab YO, Dobrobolska OV, Vovk IM, Loban’ GA. Bacterial factors of cariogenicity: literature review. Wiad Lek. 2018;71(2 pt 2):378-382.
- Ananieva MM, Faustova MO, Basarab IO, Loban’ GA. Kocuria rosea, Kocuria kristinae, Leuconostoc mesenteroides as caries-causing representatives of oral microflora. Wiad Lek. 2017;70(2 pt 2):296-298.
- Priebe S, Matanov A, Janković Gavrilović J, McCrone P, Ljubotina D, Knezević G, et al. Consequences of untreated posttraumatic stress disorder following war in former Yugoslavia: morbidity, subjective quality of life, and care costs. Croat Med J. 2009;50(5):465-475. doi: 10.3325/cmj.2009.50.465.
- Martins JR, Díaz-Fabregat B, Ramírez-Carmona W, Monteiro DR, Pessan JP, Antoniali C. Salivary biomarkers of oxidative stress in children with dental caries: systematic review and meta-analysis. Arch Oral Biol. 2022;139:105432. doi: 10.1016/j.archoralbio.2022.105432.
- Tsuber V, Kadamov Y, Tarasenko L. Activation of antioxidant defenses in whole saliva by psychosocial stress is more manifested in young women than in young men. PLoS One. 2014;9(12):e115048. doi: 10.1371/journal.pone.0115048.
- Thabet AM, Thabet SS, Vostanis P. The relationship between war trauma, PTSD, depression, and anxiety among Palestinian children in the Gaza Strip. Health Sci J. 2016;10(5):1.
- Hamid SH, Dashash MAD. The impact of post-traumatic stress disorder on dental and gingival status of children during Syrian crisis: a preliminary study. J Investig Clin Dent. 2019;10(1):e12372. doi: 10.1111/jicd.12372.
- Hamid SH, et al. Oral health-related quality of life and self-esteem of children with post traumatic stress disorder living in war zones: a case-control study. Res Sq. 2020 Jan 6. doi: 10.21203/rs.2.20107/v1.
- Adeniyi AA, Folayan MO, Arowolo O, Oziegbe EO, Chukwumah NM, El-Tantawi M. Associations between oral habits, dental an–xiety, dental service utilization, and maternal mental health status among 6- to 12-year-old children in Ile-Ife, Nigeria. Eur Arch Paediatr Dent. 2023;24(2):177-185. doi: 10.1007/s40368-022-00767-x.
- Habal W, Alkattan R, Hajeer MY, Alkhouli M, Al-Nerabieah Z, Habal T, Awawdeh M. Impact of Syrian conflict on the oral health of adolescents: a cross-sectional study. Cureus. 2024;16(2):e54613. doi: 10.7759/cureus.54613.
- Alhaffar BA, Alawabdi R, Barakat L, Kouchaji C. Oral health and socio-economic status among children during Syrian crisis: a cross-sectional study. BMC Oral Health. 2019;19(1):165. doi: 10.1186/s12903-019-0856-8.
- Abuhaloob L, Maguire A, Moynihan P. Total daily fluoride intake and the relative contributions of foods, drinks and toothpaste by 3- to 4-year-old children in the Gaza Strip — Palestine. Int J Paediatr Dent. 2015;25(2):127-135. doi: 10.1111/ipd.12108.
- Ballo L, Arheiam A, Marhazlinda J. Determinants of caries experience and the impact on the OHRQOL of 6-year-old Libyan children: a cross-sectional survey. BMC Oral Health. 2021;21:320. doi: 10.1186/s12903-021-01681-2.
- Aoun E, Ballo L, Elhabony S, Arheiam A. Association between dental caries and obesity among Libyan schoolchildren during the armed conflict in Benghazi. BMC Oral Health. 2023;23(1):44. doi: 10.1186/s12903-023-02728-2.
- Arheiam AA, Harris RV, Baker SR. Changes in dental caries and su–gar intake before and during the conflict in Libya: a natural experiment. Community Dent Oral Epidemiol. 2020;48(3):201-207. doi: 10.1111/cdoe.12526.
- Toverud G. Dental caries in Norwegian children during and after the last World War: a preliminary report. Proc R Soc Med. 1949;42(4):249-258. doi: 10.1177/003591574904200408.
- Sognnaes RF. Analysis of wartime reduction of dental ca–ries in European children; with special regard to observations in Norway. Am J Dis Child (1911). 1948;75(6):792-821. doi: 10.1001/archpedi.1948.02030020810002.
- Ballouk MA, Dashash M. Caries prevalence and dental health of 8–12 year-old children in Damascus city in Syria during the Syrian crisis: a cross-sectional epidemiological oral health survey. BMC Oral Health. 2019;19(1):16. doi: 10.1186/s12903-019-0713-9.
- Al-Otaibi MF, Al-Mamari F, Baskaradoss JK. Oral health status of 12-year-old school children in Yemen: a cross-sectional survey. Eur J Paediatr Dent. 2012;13(4):324-328.
- Ridho FM, Sofyan LBM. The relationship between family economic status and parents’ level of knowledge about dental caries disease in early childhood. Prima J Oral Dent Sci. 2023;6(1):11-17. doi: 10.34012/primajods.v6i1.3750.
- Arheiam A, Alhashani A, Kwidir T, Bosif Y, Ballo L, Tantawi ME. Untreated dental caries among Libyan children during and after the war and in internally displaced person camps. Community Dent Oral Epidemiol. 2023;51(4):636-643. doi: 10.1111/cdoe.12886.
- Cianetti S, Viarchi A, Lombardo G, Truppa CT, Shubets I, Cialfi D, et al. Real-world dental health of Ukrainian war refugee children and adolescents in Umbria, Italy: preliminary data. BMC Oral Health. 2025;25(1):512. doi: 10.1186/s12903-025-05543-z.
- Ivanković A, Lukić IK, Ivanković Z, Radić A, Vukić I, Simić A. Dental caries in postwar Bosnia and Herzegovina. Community Dent Oral Epidemiol. 2003;31(2):100-104. doi: 10.1034/j.1600-0528.2003.00052.x.
- Ahmed NA, Astrøm AN, Skaug N, Petersen PE. Dental ca–ries prevalence and risk factors among 12-year old schoolchildren from Baghdad, Iraq: a post-war survey. Int Dent J. 2007;57(1):36-44. doi: 10.1111/j.1875-595x.2007.tb00116.x.
- Kazwini R, Kasem T, Alhuda NEA, Albarshah M, Subeh D, Alhaffar MHDBA. Oral health assessment in a sample of displaced people as a result of the war in Syria in Damascus city: results of non-profit initiative. BMC Oral Health. 2021;21(1):532. doi: 10.1186/s12903-021-01874-9.
- Alshayeb L, Dashash M. Prevalence and clinical risk factors of dental caries in Syrian children: a cross-sectional study. Sci Rep. 2025;15(1):10721. doi: 10.1038/s41598-025-95534-5.
- Janković B, Ciglar I, Knezević A, Jurić H, Buković D, Stanicić T. Caries and oral hygiene in children in postwar Novi Travnik (Bosnia and Herzegovina) and Zabok (Croatia). Coll Antropol. 2004;28(1):439-445.
- Kizi G, Barata RA, Ventura I, Flores-Fraile J, Ribas-Perez D, Castaño-Seiquer A. Oral health in migrant children in Melilla, Spain. Children (Basel). 2023;10(5):888. doi: 10.3390/children10050888.
- Riatto SG, Montero J, Pérez DR, Castaño-Seiquer A, Dib A. Oral health status of Syrian children in the refugee center of Melilla, Spain. Int J Dent. 2018;2018:2637508. doi: 10.1155/2018/2637508.
- Youssefi MA, Afroughi S. Prevalence and associated factors of dental caries in primary schoolchildren: an Iranian setting. Int J Dent. 2020;2020:8731486. doi: 10.1155/2020/8731486.
- Abuhaloob L, Petersen PE. Oral health status among children and adolescents in governmental and private schools of the Palestinian Territories. Int Dent J. 2018;68(2):105-112. doi: 10.1111/idj.12345.
- Sheshukova O, Mosiienko AS, Polishchuk TV, Maksymenko AI, Marchenko AV, Bauman SS, Lokhmatova NM. Comprehensive assessment of caries resistance in 6–7 year-old children residing in Poltava and internally displaced children. Wiad Lek. 2024;77(12):2487-2492. doi: 10.36740/WLek/197114.
- Tikhonova S, Booij L, D’Souza V, Crosara KTB, Siqueira WL, Emami E. Investigating the association between stress, saliva and dental caries: a scoping review. BMC Oral Health. 2018;18(1):41. doi: 10.1186/s12903-018-0500-z.