Журнал «Здоровье ребенка» Том 20, №2, 2025
Вернуться к номеру
Автозапальні захворювання. Частина 3: NLRP та NLRC інфламасомопатії. Біологічна терапія інфламасомопатій
Авторы: Шварацька О.В., Бордій Т.А., Калічевська М.В., Клименко О.В., Таран О.М., Клімова О.В., Віленський Я.В., Мавропуло Т.К.
Дніпровський державний медичний університет, м. Дніпро, Україна
Рубрики: Педиатрия/Неонатология
Разделы: Справочник специалиста
Версия для печати
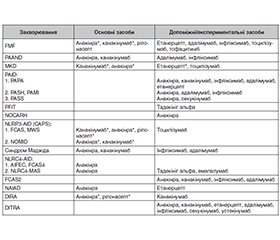
Інфламасомопатії та інші синдроми посилення сигналу інтерлейкіну (IL)-1 є значущим кластером системних автозапальних захворювань (САЗЗ) — моногенних станів, які характеризуються епізодичним спонтанним полісистемним запаленням, що виникає переважно через невідповідну активацію антиген-незалежних запальних механізмів без участі автоантитіл, тобто опосередковується механізмами вродженого імунітету. Автозапалення наразі розглядається як окрема категорія імунної дисфункції поряд з автоімунітетом/алергією та імунодефіцитом. Цей науковий огляд є третім у серії публікацій, об’єднаних загальною метою підвищення обізнаності лікарів про діагностику та менеджмент САЗЗ у дітей. В огляді висвітлені імунобіологічні особливості інфламасом, які містять білки з нуклеотидзв’язувальним доменом, що містять повтори з високим вмістом лейцину (NLR), та надана клініко-патогенетична характеристика генетично визначених NLRP3-, NLRP12-, NLRP1- та NLRC4-асоційованих інфламасомопатій. Окрім цього, в роботі обговорено потенціал таргетної біологічної терапії інфламасомопатій, що ґрунтується на молекулярному імунопатогенезі захворювання і яка наразі вважається ключовим напрямом лікування САЗЗ. Також нами було узагальнено сучасний досвід використання специфічних біологічних препаратів у терапії окремих інфламасомопатій, а саме засобів, спрямованих на блокаду ефектів IL-1, IL-6, IL-17, IL-12/23, інтерферону-гамма, фактора некрозу пухлини тощо. Пошук інформації за останні 10 років здійснювався по базах даних Web of Science, Scopus, PubMed Central®, Google Scholar за ключовими словами: autoinflammatory diseases, autoinflammation, inflammasomopathies, NLRP, NLRC, biologic therapies.
Inflammasomopathies and other enhanced interleukin (IL)-1 signaling syndromes represent a significant cluster of systemic autoinflammatory diseases (SAIDs) which are monogenic disorders characterized by episodic spontaneous multisystemic inflammation mediated by innate immunity and resulting mainly from inappropriate activation of antigen-independent inflammatory mechanisms without production of autoantibodies. Autoinflammation is currently considered a distinct category of immune dysfunction along with autoimmunity/allergy and immunodeficiency. This scientific review is the third in a series of publications aimed at raising awareness among healthcare professionals regarding the diagnosis and management of SAIDs in children. The review highlights the immunobiological features of inflammasomes containing nucleotide-binding domain, leucine-rich repeat-containing proteins (NLRs). It also presents the clinical and pathogenetic features of the currently genetically defined NLRP3-, NLRP12-, NLRP1- and NLRC4-associated inflammasomopathies. The paper also discusses the potential of biologic-targeted therapies for inflammasomopathies which are now considered a key trend in the treatment of SAIDs and based on the molecular immunopathogenesis of the disease. Furthermore, we summarized the current experience of using available biological agents in the treatment of specific inflammasomopathies, namely agents blocking the effects of IL-1, IL-6, IL-17, IL-12/23, interferon-gamma, and tumor necrosis factor. Data were collected through a focused search over the Web of Science, Scopus, PubMed Central®, Google Scholar databases for the past 10 years using the keywords “autoinflammatory diseases”, “autoinflammation”, “inflammasomopathies”, “NLRP”, “NLRC”, “biologic therapies”.
автозапальні захворювання; інфламасомопатії; інтерлейкін 1; біологічні препарати; терапія; огляд
autoinflammatory diseases; inflammasomopathies; interleukin 1; biologics; treatment; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Krainer J, Siebenhandl S, Weinhäusel A. Systemic autoinflammatory diseases. J Autoimmun. 2020 May;109:102421. doi: 10.1016/j.jaut.2020.102421.
- Havnaer A, Han G. Autoinflammatory Disorders: A Review and Update on Pathogenesis and Treatment. Am J Clin Dermatol. 2019 Aug;20(4):539-564. doi: 10.1007/s40257-019-00440-y.
- Николаєнко В.Б. Алергічні хвороби та автоімунні стани у дітей — сучасні підходи до діагностики та лікування. Укр. мед. часопис. 2020;1(135):38-45.
- Rood JE, Behrens EM. Inherited Autoinflammatory Syndromes. Annu Rev Pathol. 2022 Jan 24;17:227-249. doi: 10.1146/annurev-pathmechdis-030121-041528.
- De Jesus AA, Goldbach-Mansky R. Genetically defined autoinflammatory diseases. Oral Dis. 2016 Oct;22(7):591-604. doi: 10.1111/odi.12448.
- Hoffman HM, Broderick L. The role of the inflammasome in patients with autoinflammatory diseases. J Allergy Clin Immunol. 2016 Jul;138(1):3-14. doi: 10.1016/j.jaci.2016.05.001.
- Nigrovic PA, Lee PY, Hoffman HM. Monogenic autoinflammatory disorders: Conceptual overview, phenotype, and clinical approach. J Allergy Clin Immunol. 2020 Nov;146(5):925-937. doi: 10.1016/j.jaci.2020.08.017.
- Lin B, Goldbach-Mansky R. Pathogenic insights from genetic causes of autoinflammatory inflammasomopathies and interferonopathies. J Allergy Clin Immunol. 2022 Mar;149(3):819-832. doi: 10.1016/j.jaci.2021.10.027.
- Maalouly M, Saade S, Kurban M. Autoinflammatory diseases: what is behind them and what is new? Dermatol Reports. 2022 Dec 29;15(2):9625. doi: 10.4081/dr.2023.9625.
- Davis BK, Wen H, Ting JP. The inflammasome NLRs in immunity, inflammation, and associated diseases. Annu Rev Immunol. 2011;29:707-35. doi: 10.1146/annurev-immunol-031210-101405.
- Zheng D, Liwinski T, Elinav E. Inflammasome activation and regulation: toward a better understanding of complex mechanisms. Cell Discov. 2020 Jun 9;6:36. doi: 10.1038/s41421-020-0167-x.
- Alehashemi S, Goldbach-Mansky R. Human Autoinflammatory Diseases Mediated by NLRP3-, Pyrin-, NLRP1-, and NLRC4-Inflammasome Dysregulation Updates on Diagnosis, Treatment, and the Respective Roles of IL-1 and IL-18. Front Immunol. 2020 Aug 25;11:1840. doi: 10.3389/fimmu.2020.01840.
- La Bella S, Di Ludovico A, Di Donato G, et al. The pyrin inflammasome, a leading actor in pediatric autoinflammatory diseases. Front Immunol. 2024 Jan 5;14:1341680. doi: 10.3389/fimmu.2023.1341680.
- Li Y, Yu M, Lu M. Pathophysiology, clinical manifestations and current management of IL-1 mediated monogenic systemic autoinflammatory diseases, a literature review. Pediatr Rheumatol Online J. 2022 Oct 17;20(1):90. doi: 10.1186/s12969-022-00728-0.
- Akdis M, Aab A, Altunbulakli C, et al. Interleukins (from IL-1 to IL-38), interferons, transforming growth factor β, and TNF-α: Receptors, functions, and roles in diseases. J Allergy Clin Immunol. 2016 Oct;138(4):984-1010. doi: 10.1016/j.jaci.2016.06.033.
- Zhou L, Todorovic V. Interleukin-36: Structure, Signaling and Function. Adv Exp Med Biol. 2021;21:191-210. doi: 10.1007/5584_2020_488.
- Hikima J, Morimoto N. Evolutive aspects of inflammasomes. In: Pelegrin P, editor. Inflammasome Biology. Academic Press. 2023:235-245. doi: 10.1016/B978-0-323-91802-2.00013-X.
- Schnappauf O, Chae JJ, Kastner DL, Aksentijevich I. The Pyrin Inflammasome in Health and Disease. Front Immunol. 2019 Aug 7;10:1745. doi: 10.3389/fimmu.2019.01745.
- Motta V, Soares F, Sun T, Philpott DJ. NOD-like receptors: versatile cytosolic sentinels. Physiol Rev. 2015 Jan;95(1):149-78. doi: 10.1152/physrev.00009.2014.
- Yang Y, Wang H, Kouadir M, Song H, Shi F. Recent advances in the mechanisms of NLRP3 inflammasome activation and its inhibitors. Cell Death Dis. 2019 Feb 12;10(2):128. doi: 10.1038/s41419-019-1413-8.
- Zhang J, Lee PY, Aksentijevich I, Zhou Q. How to Build a Fire: The Genetics of Autoinflammatory Diseases. Annu Rev Genet. 2023 Nov 27;57:245-274. doi: 10.1146/annurev-genet-030123-084224.
- Kawakami A, Endo Y, Koga T, Yoshiura KI, Migita K. Autoinflammatory disease: clinical perspectives and therapeutic strategies. Inflamm Regen. 2022 Dec 2;42(1):37. doi: 10.1186/s41232-022-00217-7.
- Xu Z, Kombe Kombe AJ, Deng S, et al. NLRP inflammasomes in health and disease. Mol Biomed. 2024 Apr 22;5(1):14. doi: 10.1186/s43556-024-00179-x.
- Bauer R, Rauch I. The NAIP/NLRC4 inflammasome in infection and pathology. Mol Aspects Med. 2020 Dec;76:100863. doi: 10.1016/j.mam.2020.100863.
- Kay C, Wang R, Kirkby M, Man SM. Molecular mechanisms activating the NAIP-NLRC4 inflammasome: Implications in infectious di–sease, autoinflammation, and cancer. Immunol Rev. 2020 Sep;297(1):67-82. doi: 10.1111/imr.12906.
- Tuladhar S, Kanneganti TD. NLRP12 in innate immunity and inflammation. Mol Aspects Med. 2020 Dec;76:100887. doi: 10.1016/j.mam.2020.100887.
- Tuncer S, Fiorillo MT, Sorrentino R. The multifaceted nature of NLRP12. J Leukoc Biol. 2014 Dec;96(6):991-1000. doi: 10.1189/jlb.3RU0514-265RR.
- Wang HF. NLRP12-associated systemic autoinflammatory diseases in children. Pediatr Rheumatol Online J. 2022 Feb 5;20(1):9. doi: 10.1186/s12969-022-00669-8.
- Yu CH, Moecking J, Geyer M, Masters SL. Mechanisms of –NLRP1-Mediated Autoinflammatory Disease in Humans and Mice. J Mol Biol. 2018 Jan 19;430(2):142-152. doi: 10.1016/j.jmb.2017.07.012.
- Flemming A. Functional degradation ignites the inflammasome. Nat Rev Immunol. 2019 Jun;19(6):349. doi: 10.1038/s41577-019-0169-9.
- Chui AJ, Okondo MC, Rao SD, et al. N-terminal degradation activates the NLRP1B inflammasome. Science. 2019 Apr 5;364(6435):82-85. doi: 10.1126/science.aau1208.
- Eldeeb MA, Fahlman RP, Esmaili M, Fon EA. When Degradation Elicits the Alarm: N-Terminal Degradation of NLRP1B Unleashes Its Inflammasome Activity. Mol Cell. 2019 May 16;74(4):637-639. doi: 10.1016/j.molcel.2019.04.032.
- Sandstrom A, Mitchell PS, Goers L, et al. Functional degradation: A mechanism of NLRP1 inflammasome activation by diverse pathogen enzymes. Science. 2019 Apr 5;364(6435):eaau1330. doi: 10.1126/science.aau1330.
- Moghaddas F. Monogenic autoinflammatory disorders: beyond the periodic fever. Intern Med J. 2020 Feb;50(2):151-164. doi: 10.1111/imj.14414.
- Zhong FL, Robinson K, Teo DET, et al. Human DPP9 represses NLRP1 inflammasome and protects against autoinflammatory diseases via both peptidase activity and FIIND domain binding. J Biol Chem. 2018 Dec 7;293(49):18864-18878. doi: 10.1074/jbc.RA118.004350.
- Ben-Chetrit E, Gattorno M, Gul A, et al. Consensus proposal for taxonomy and definition of the autoinflammatory diseases (AIDs): a Delphi study. Ann Rheum Dis. 2018 Nov;77(11):1558-1565. doi: 10.1136/annrheumdis-2017-212515.
- Almeida de Jesus A, Goldbach-Mansky R. Monogenic autoinflammatory diseases: concept and clinical manifestations. Clin Immunol. 2013 Jun;147(3):155-74. doi: 10.1016/j.clim.2013.03.016.
- Ito S, Hara Y, Kubota T. CARD8 is a negative regulator for NLRP3 inflammasome, but mutant NLRP3 in cryopyrin-associated periodic syndromes escapes the restriction. Arthritis Res Ther. 2014 Feb 12;16(1):R52. doi: 10.1186/ar4483.
- Боярчук О.Р., Волянська Л.А., Ковальчук Т.А., Кінаш М.І. Артрити при первинних імунодефіцитах. Біль. Суглоби. Хребет. 2017;7:15-20. doi: 10.22141/2224-1507.7.1.2017.102433
- Зайков С.В., Богомолов А.Є., Кириленко Т.В., Гришило А.П. Гостра кропив’янка — актуальна мультидисциплінарна проблема: огляд літератури. Астма та алергія. 2022;3:66-76. doi: 10.31655/2307-3373-2022-3-66-76.
- Gattorno M, Hofer M, Federici S, et al. Classification criteria for autoinflammatory recurrent fevers. Ann Rheum Dis. 2019 Aug;78(8):1025-1032. doi: 10.1136/annrheumdis-2019-215048.
- Federici S, Sormani MP, Ozen S, et al. Evidence-based provisional clinical classification criteria for autoinflammatory periodic fevers. Ann Rheum Dis. 2015 May;74(5):799-805. doi: 10.1136/annrheumdis-2014-206580.
- Romano M, Arici ZS, Piskin D, et al. The 2021 EULAR/American College of Rheumatology Points to Consider for Diagnosis, Management and Monitoring of the Interleukin-1 Mediated Autoinflammatory Diseases: Cryopyrin-Associated Periodic Syndromes, Tumour Necrosis Factor Receptor-Associated Periodic Syndrome, Mevalonate Kinase Deficiency, and Deficiency of the Interleukin-1 Receptor Antagonist. Arthritis Rheumatol. 2022 Jul;74(7):1102-1121. doi: 10.1002/art.42139.
- Moltrasio C, Romagnuolo M, Marzano AV. NLRP3 inflammasome and NLRP3-related autoinflammatory diseases: From cryopyrin function to targeted therapies. Front Immunol. 2022 Oct 6;13:1007705. doi: 10.3389/fimmu.2022.1007705.
- Lordén G, Sanjuán-García I, de Pablo N, et al. Lipin-2 regulates NLRP3 inflammasome by affecting P2X7 receptor activation. J Exp Med. 2017 Feb;214(2):511-528. doi: 10.1084/jem.20161452.
- Chavan PP, Aksentijevich I, Daftary A, et al. Majeed Syndrome: Five Cases With Novel Mutations From Unrelated Families in India With a Review of Literature. J Rheumatol. 2021 Dec;48(12):1850-1855. doi: 10.3899/jrheum.201663.
- An J, Marwaha A, Laxer RM. Autoinflammatory Diseases: A Review. J Rheumatol. 2024 Sep 1;51(9):848-861. doi: 10.3899/jrheum.2023-1209.
- Knop J, Spilgies LM, Rufli S, et al. TNFR2 induced priming of the inflammasome leads to a RIPK1-dependent cell death in the absence of XIAP. Cell Death Dis. 2019 Sep 20;10(10):700. doi: 10.1038/s41419-019-1938-x.
- Mudde ACA, Booth C, Marsh RA. Evolution of Our Understanding of XIAP Deficiency. Front Pediatr. 2021 Jun 17;9:660520. doi: 10.3389/fped.2021.660520.
- Cuny GD, Degterev A. RIPK protein kinase family: Atypical lives of typical kinases. Semin Cell Dev Biol. 2021 Jan;109:96-105. doi: 10.1016/j.semcdb.2020.06.014.
- Volker-Touw CM, de Koning HD, Giltay JC, et al. Erythematous nodes, urticarial rash and arthralgias in a large pedigree with NLRC4-related autoinflammatory disease, expansion of the phenotype. Br J Dermatol. 2017 Jan;176(1):244-248. doi: 10.1111/bjd.14757.
- Asna Ashari K, Parvaneh N, Mirnia K, et al. Three cases of autoinflammatory disease with novel NLRC4 mutations, and the first mutation reported in the CARD domain of NLRC4 associated with autoinflammatory infantile enterocolitis (AIFEC). Pediatr Rheumatol Online J. 2024 Oct 18;22(1):90. doi: 10.1186/s12969-024-01020-z.
- Wang L, Wen W, Deng M, et al. A Novel Mutation in the NBD Domain of NLRC4 Causes Mild Autoinflammation With Recurrent Urticaria. Front Immunol. 2021 Jun 23;12:674808. doi: 10.3389/fimmu.2021.674808.
- Wang J, Ye Q, Zheng W, et al. Low-ratio somatic NLRC4 mutation causes late-onset autoinflammatory disease. Ann Rheum Dis. 2022 Aug;81(8):1173-1178. doi: 10.1136/annrheumdis-2021-221708.
- Canna SW, Goldbach-Mansky R. New monogenic autoinflammatory diseases — a clinical overview. Semin Immunopathol. 2015 Jul;37(4):387-94. doi: 10.1007/s00281-015-0493-5.
- Sztajnbok F, Fonseca AR, Campos LR, et al. Hemophagocytic lymphohistiocytosis and macrophage activation syndrome: two rare sides of the same devastating coin. Adv Rheumatol. 2024 Apr 16;64(1):28. doi: 10.1186/s42358-024-00370-2.
- Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell. 2002 Aug;10(2):417-26. doi: 10.1016/s1097-2765(02)00599-3.
- Sureja NP, Rajasekhar L. Autoinflammation with Arthritis and Dyskeratosis an Inflammasomopathy: Case Report and Review of Literature. Indian Journal of Rheumatology. 2022 March;17(1):65-68. doi: 10.4103/injr.injr_17_21.
- Grandemange S, Sanchez E, Louis-Plence P, et al. A new autoinflammatory and autoimmune syndrome associated with NLRP1 mutations: NAIAD (NLRP1-associated autoinflammation with arthritis and dyskeratosis). Ann Rheum Dis. 2017 Jul;76(7):1191-1198. doi: 10.1136/annrheumdis-2016-210021.
- Burian M, Yazdi AS. NLRP1 Is the Key Inflammasome in Primary Human Keratinocytes. J Invest Dermatol. 2018 Dec;138(12):2507-2510. doi: 10.1016/j.jid.2018.08.004.
- Harapas CR, Robinson KS, Lay K, et al. DPP9 deficiency: An inflammasomopathy that can be rescued by lowering NLRP1/IL-1 signaling. Sci Immunol. 2022 Sep 16;7(75):eabi4611. doi: 10.1126/sciimmunol.abi4611.
- Özen S, Batu ED, Demir S. Familial Mediterranean Fever: Recent Developments in Pathogenesis and New Recommendations for Management. Front Immunol. 2017 Mar 23;8:253. doi: 10.3389/fimmu.2017.00253.
- Park YH, Wood G, Kastner DL, Chae JJ. Pyrin inflammasome activation and RhoA signaling in the autoinflammatory diseases FMF and HIDS. Nat Immunol. 2016 Aug;17(8):914-21. doi: 10.1038/ni.3457.
- Wang Y, Wang J, Zheng W, et al. Identification of an IL-1 receptor mutation driving autoinflammation directs IL-1-targeted drug design. Immunity. 2023 Jul 11;56(7):1485-1501.e7. doi: 10.1016/j.immuni.2023.05.014.
- Ozen S. Update in familial Mediterranean fever. Curr Opin Rheumatol. 2021 Sep 1;33(5):398-402. doi: 10.1097/BOR.0000000000000821.
- Ozen S, Demirkaya E, Erer B, et al. EULAR recommendations for the management of familial Mediterranean fever. Ann Rheum Dis. 2016 Apr;75(4):644-51. doi: 10.1136/annrheumdis-2015-208690.
- Kul Cinar O, Putland A, Wynne K, Eleftheriou D, Brogan PA. Hereditary Systemic Autoinflammatory Diseases: Therapeutic Stratification. Front Pediatr. 2022 Apr 28;10:867679. doi: 10.3389/fped.2022.867679.
- Bettiol A, Lopalco G, Emmi G, et al. Unveiling the Efficacy, Safety, and Tolerability of Anti-Interleukin-1 Treatment in Monogenic and Multifactorial Autoinflammatory Diseases. Int J Mol Sci. 2019 Apr 17;20(8):1898. doi: 10.3390/ijms20081898.
- Grattagliano I, Bonfrate L, Ruggiero V, et al. Novel therapeutics for the treatment of familial Mediterranean fever: from colchicine to biologics. Clin Pharmacol Ther. 2014 Jan;95(1):89-97. doi: 10.1038/clpt.2013.148.
- Ter Haar NM, Oswald M, Jeyaratnam J, et al. Recommendations for the management of autoinflammatory diseases. Ann Rheum Dis. 2015 Sep;74(9):1636-44. doi: 10.1136/annrheumdis-2015-207546.
- De Benedetti F, Gattorno M, Anton J, et al. Canakinumab for the Treatment of Autoinflammatory Recurrent Fever Syndromes. N Engl J Med. 2018 May 17;378(20):1908-1919. doi: 10.1056/NEJMoa1706314.
- Garg M, de Jesus AA, Chapelle D, et al. Rilonacept maintains long-term inflammatory remission in patients with deficiency of the IL-1 receptor antagonist. JCI Insight. 2017 Aug 17;2(16):e94838. doi: 10.1172/jci.insight.94838.
- Cebeci SO, Yildiz M, Gunalp A, et al. The efficacy of a single-dose anakinra injection during disease attack in pediatric familial Mediterranean fever. Rheumatol Int. 2024 Nov;44(11):2569-2575. doi: 10.1007/s00296-023-05351-0.
- Moghaddas F, Llamas R, De Nardo D, et al. A novel Pyrin-Associated Autoinflammation with Neutrophilic Dermatosis mutation further defines 14-3-3 binding of pyrin and distinction to Familial Mediterranean Fever. Ann Rheum Dis. 2017 Dec;76(12):2085-2094. doi: 10.1136/annrheumdis-2017-211473.
- Roy NBA, Zaal AI, Hall G, et al. Majeed syndrome: description of a novel mutation and therapeutic response to bisphosphonates and IL-1 blockade with anakinra. Rheumatology (Oxford). 2020 Feb 1;59(2):448-451. doi: 10.1093/rheumatology/kez317.
- Kırmızıer G, Kılınç EA, Yıldırım NO, Türsen Ü. Successful treatment of PASS syndrome with IVIG and anti-IL-1 treatment: A case report. Int J Rheum Dis. 2024 Mar;27(3):e15114. doi: 10.1111/1756-185X.15114.
- Hospach T, Glowatzki F, Blankenburg F, et al. Scoping review of biological treatment of deficiency of interleukin-36 receptor antagonist (DITRA) in children and adolescents. Pediatr Rheumatol Online J. 2019 Jul 8;17(1):37. doi: 10.1186/s12969-019-0338-1.
- Canna SW, Girard C, Malle L, et al. Life-threatening NLRC4-associated hyperinflammation successfully treated with IL-18 inhibition. J Allergy Clin Immunol. 2017 May;139(5):1698-1701. doi: 10.1016/j.jaci.2016.10.022.
- Wang Y, Wu N, Yu K, Shen M. Case Report: Pyogenic Arthritis, Pyoderma Gangrenosum, and Acne: A Single-Center Experience and Literature Review. Front Immunol. 2021 Oct 22;12:735851. doi: 10.3389/fimmu.2021.735851.
- El Hasbani G, Jawad A, Uthman I. Update on the management of colchicine resistant Familial Mediterranean Fever (FMF). Orphanet J Rare Dis. 2019 Oct 15;14(1):224. doi: 10.1186/s13023-019-1201-7.
- Koryllou A, Mejbri M, Theodoropoulou K, Hofer M, Carlomagno R. Chronic Nonbacterial Osteomyelitis in Children. Children (Basel). 2021 Jun 25;8(7):551. doi: 10.3390/children8070551.
- Li M, Xiang H, Liang Y, Xue L, et al. Secukinumab for PASS syndrome: A new choice for therapeutic challenge? Dermatol Ther. 2022 Jul;35(7):e15507. doi: 10.1111/dth.15507.
- Hausmann JS. Targeting cytokines to treat autoinflammatory diseases. Clin Immunol. 2019 Sep;206:23-32. doi: 10.1016/j.clim.2018.10.016.
- Rafiq NK, Lachmann H, Joensen F, Herlin T, Brogan PA. Tocilizumab for the Treatment of Mevalonate Kinase Deficiency. Case Rep Pediatr. 2018 Aug 26;2018:3514645. doi: 10.1155/2018/3514645.
- Han JH, Je YJ, Yoon HJ, et al. The First Case Series of Cryopyrin-Associated Periodic Syndrome in Korea. Allergy Asthma Immunol Res. 2019 Jul;11(4):583-588. doi: 10.4168/aair.2019.11.4.583.
- Hu X, Li J, Fu M, Zhao X, Wang W. The JAK/STAT signaling pathway: from bench to clinic. Signal Transduct Target Ther. 2021 Nov 26;6(1):402. doi: 10.1038/s41392-021-00791-1.
- Carapito R, Carapito C, Morlon A, et al. Multi-OMICS analyses unveil STAT1 as a potential modifier gene in mevalonate kinase deficiency. Ann Rheum Dis. 2018 Nov;77(11):1675-1687. doi: 10.1136/annrheumdis-2018-213524.
- Marino A, Tirelli F, Giani T, Cimaz R. Periodic fever syndromes and the autoinflammatory diseases (AIDs). J Transl Autoimmun. 2019 Dec 17;3:100031. doi: 10.1016/j.jtauto.2019.100031.
- Coll RC, Schroder K, Pelegrín P. NLRP3 and pyroptosis blo–ckers for treating inflammatory diseases. Trends Pharmacol Sci. 2022 Aug;43(8):653-668. doi: 10.1016/j.tips.2022.04.003.
- Dai Z, Liu WC, Chen XY, et al. Gasdermin D-mediated pyroptosis: mechanisms, diseases, and inhibitors. Front Immunol. 2023 May 18;14:1178662. doi: 10.3389/fimmu.2023.1178662.