Журнал «Медицина неотложных состояний» Том 20, №7, 2024
Вернуться к номеру
Особливості патогенезу бойової травми
Авторы: Макаров В.В. (1, 2), Негодуйко В.В. (1, 2), Феськов В.М. (1), Петюнін О.Г. (1), Смоляник К.М. (1), Сизий М.Ю. (1)
(1) - Харківський національний медичний університет, м. Харків, Україна
(2) - Військово-медичний клінічний центр Північного регіону, м. Харків, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
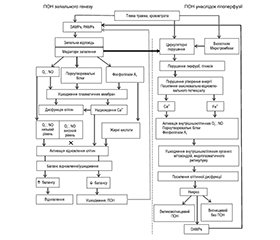
Світова тенденція військової хірургії останніх десятиліть — поліпшення результатів лікування бойової травми, зниження як ранньої, так і пізньої летальності, що пов’язують з навчанням учасників бойових дій надання першої медичної допомоги, самодопомоги, поліпшенням медичної логістики, упровадженням принципів хірургії контролю ушкоджень і ранньої ресусцитації, етапністю допомоги. Однак у структурі летальності, особливо пізньої, провідні позиції, як і раніше, посідають гостре ушкодження легень, гострий респіраторний дистрес-синдром, поліорганна недостатність, патогенезу яких і присвячено цей огляд. Понятійний інструмент даного огляду виходить за межі звичайного хірургічного. Однак як бойова травма потребує мультисистемного підходу, так і проблема поліорганної недостатності може бути вирішена лише при взаємодії різних дисциплін, тому лише такий рівень розуміння відкриває перспективу подальшого розвитку.
The world trend of military surgery of last decades is an improvement of treatment outcomes in combat trauma, the reduction of both early and late mortality, which is associated with the training of combatants in providing first aid, self-help, improving medical logistics, implementing the principles of damage control surgery and early resuscitation, staging of assistance. However, in the structure of mortality, especially late, the leading positions, as before, belong to acute lung damage, acute respiratory distress syndrome, multiple organ failure whose pathogenesis is considered in this review. The conceptual tool of this study goes beyond the usual surgical one. However, just as combat trauma requires a multisystem approach, so the solution to the problem of multiple organ failure can be found only with the interaction of various disciplines, and therefore only this level of understanding of this problem opens the prospect of further development.
бойова травма; поліорганна недостатність; патогенез
combat trauma; multiple organ failure; pathogenesis
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Instructions on military field surgery / edited by K.V. Gumenyuka, S.O. Korolya. It was dying. Kyiv: Lyudmila Publishing House, 2024. 572 p.
- Lee CC, Marill KA, Carter WA, Crupi RS. A current concept of trauma-induced multiorgan failure. Ann Emerg Med. 2001;38(2):170-176.
- Dufour-Gaume F, Frescaline N, Cardona V, Prat NJ. Danger Signals in Traumatic Hemorrhagic Shock and New Lines for Clinical Applications. Frontiers in Physiology. 2023;13.
- Jason H, Waseem M, David F. Trauma primary survey [Електронний ресурс]. StatPearls. 2023;10. https://www.ncbi.nlm.nih.gov/books/NBK430800.
- Osterweis M, Kleinman А, Mechanic D. Pain and Disability: Clinical, Behavioral, and Public Policy Perspectives. Washington: National Academies Press (US), 1987. 450 р.
- Guyton A, Hall H. Textbook of Medical Physiology. Philadelphia: PA: Saunders, 2006. 350 p.
- Pruitt BA Jr, Mason AD Jr, Moncrief JA. Hemodynamic changes in the early postburn patient: the influence of fluid administration and of a vasodilator (hydralazine). J Trauma. 1971;11(1):36-46.
- Kelly JF, Ritenour AE, McLaughlin DF, et al. Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003–2004 versus 2006. J Trauma. 2008;64:S21-27.
- Cannon JW. Hemorrhagic Shock. N Engl J Med. 2018;378:370-379
- Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14:30-38.
- Moore EE, Knudson MM, Burlew CC, et al.; WTA Study Group. Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. J Trauma. 2011;70(2):334-339.
- Chaudry IH. Cellular mechanisms in shock and ischemia and their correction. Am J Physiol. 1983;245:R117-R134.
- Ekeloef NP, Eriksen J, Kancir CB. Evaluation of two methods to calculate p50 from a single blood sample. Acta Anaesthesiol Scand. 2001;45:550-552.
- Srinivasan AJ, Morkane C, Martin DS, Welsby IJ. Should modulation of p50 be a therapeutic target in the critically ill? Expert Rev Hematol. 2017;10:449-458.
- Barbee RW, Reynolds PS, Ward KR. Assessing shock resuscitation strategies by oxygen debt repayment. Shock. 2010;33:113-22.
- Michel CC, Arkill KP, Curry FRE. The Revised Starling Principle and Its Relevance to Perioperative Fluid Management. In: Perioperative Fluid Management. Springer International Publishing, 2020.
- Matzinger P. Tolerance, danger, and the extended family. Annu Rev Immunol. 1994;12:991-1045.
- Тaanman JW. The mitochondrial genome: structure, transcription, translation and replication. Biochim Biophys Acta. 1999;1410:103-23.
- Janeway CA Jr. Approaching the asymptote? Evolution and revolution in immunology. Cold Spring Harb Symp Quant Biol. 1989;54(Pt 1):1-13.
- Takeshi Tsukamoto, R. Savanh Chanthaphavong, Hans-Christoph Pape. Current theories on the pathophysiology of multiple organ failure after trauma. Injury. 2010;41:21-6.
- Hazeldine J, Hampson P, Lord JM. The impact of trauma on neutrophil function. Injury. 2014;45(12):1824-1833.
- Xiao W, Mindrinos MN, Seok J, et al. A genomic storm in critically injured humans. The Journal of Experimental Medicine. 2011;208(13):2581-2590.
- Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2018 Jan 23;9(6):7204-7218.
- Khakpour S, Wilhelmsen K, Hellman J. Vascular endothelial cell Toll-like receptor pathways in sepsis. Innate Immun. 2015; 21:827-46.
- Tracey KJ. The inflammatory reflex. Nature. 2002;420:853-859.
- Lu H, Wen D, Wang X, et al. Host genetic variants in sepsis risk: a field synopsis and meta-analysis. Crit Care. 2019;23(1):26.
- Thayer JF, Sternberg EM. Neural aspects of immunomodulation: focus on the vagus nerve. Brain Behav Immun. 2010;24:1223-1228.
- Kozar RA, Peng Z, Zhang R, Holcomb JB, Pati S, Park P, Ko TC, Paredes A. Plasma restoration of endothelial glycocalyx in a rodent model of hemorrhagic shock. Anesth Analg. 2011;112:1289-1295.
- Reitsma S, Slaaf DW, Vink H, van Zandvoort MA, oude Egbrink MG. The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch. 2007;454:345-59.
- Pizzorno J, Murray M. Textbook of Natural Medicin. Fifth Edition. 2020. 545 р.
- Nam EJ, Park PW. Shedding of cell membrane-bound proteoglycans. Methods Mol Biol. 2012;836:291-305.
- Barelli S, Alberio L. The Role of Plasma Transfusion in Massive Bleeding: Protecting the Endothelial Glycocalyx? Front Med (Lausanne). 2019;5:91.
- Zeng Y, Zhang XF, Fu BM, Tarbell JM. The Role of Endothelial Surface Glycocalyx in Mechanosensing and Transduction. Adv Exp Med Biol. 2018;1097:1-27.
- Gouverneur M, van den Berg B, Nieuwdorp M, et al. Vasculoprotective properties of the endothelial glycocalyx: effects of fluid shear stress. J Intern Med. 2006;259:393-400.
- Haywood-Watson RJ, Holcomb JB, Gonzalez EA, Peng Z, Pati S, Park PW et al. Modulation of syndecan-1 shedding after he-morrhagic shock and resuscitation. PLoS One. 2011;6:e23530.
- Becker BF, Jacob M, Leipert S, Salmon AH, Chappell D. Degradation of the endothelial glycocalyx in clinical settings: searching for the sheddases. Br J Clin Pharmacol. 2015;80:389-402.
- Frydland M, Ostrowski SR, Møller JE, Hadziselimovic E, Holmvang L, Ravn HB, et al. Plasma Concentration of Biomarkers Reflecting Endothelial Cell- and Glycocalyx Damage are Increased in Patients With Suspected ST-Elevation Myocardial Infarction Complicated by Cardiogenic Shock. Shock. 2018;50:538-544.
- Ostrowski SR, Haase N, Müller RB, Møller MH, Pott FC, Perner A, Johansson PI. Association between biomarkers of endothelial injury and hypocoagulability in patients with severe sepsis: a prospective study. Crit Care. 2015;19:191.
- Han J, Ulevitch RJ. Limiting inflammatory responses during activation of innate immunity. Nat Immunol. 2005;6:1198-1205.
- Hofmann N, Zipperle J, Jafarmadar M, et al. Experimental models of endotheliopathy: impact of shock severity. ingentaconnect.com, 2018. https://www.ingentaconnect.com/content/wk/shk/2018/00000049/00000005/art00012.
- Xu L, Yu WK, Lin ZL, et al. Chemical sympathectomy attenuates inflammation, glycocalyx shedding and coagulation disorders in rats with acute traumatic coagulopathy. Blood Coagul Fibrinolysis. 2015;26:152-160.
- Johansson PI, Henriksen HH, Stensballe J, Gybel-Brask M, Cardenas JC, Baer LA et al. Traumatic endotheliopathy: A prospective observational study of 424 severely injured patients. Ann Surg. 2017;265(3):597-603.
- Papea H-C, Moore EE, McKinleyc T, Sauaia A. Pathophysiology in patients with polytrauma. Injury. 2022;53:2400-2412.
- Chakraborty RK, Burns B. Systemic Inflammatory Response Syndrome. StatPearls, 2020.
- Nuytinck HK, Xavier JM, Offermans W, et al. Whole-body inflammation in trauma patients: an autopsy study. Arch Surg 1988;123:1519-1524.
- Pape HC, Remmers D, Kleemann W, Goris JA, Regel G, Tscherne H. Posttraumatic multiple organ failure — a report on clinical and autopsy findings. Shock. 1994 Sep;2(3):228-34.
- Kozar RA, Pati S. Syndecan-1 restitution by plasma after hemorrhagic shock. J Trauma Acute Care Surg. 2015;78(6 Suppl 1):S83-S86.
- Borgman M, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, Sebesta J, Jenkins D, Wade CE, Hol-
- comb JB. Blood product replacement affects survival in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63:805-813.
- Mitroulis I, Alexaki VI, Kourtzelis I, Ziogas A, Hajishengallis G, Chavakis T. Leukocyte integrins: role in leukocyte recruitment and as therapeutic targets in inflammatory disease. Pharmacology & Therapeutics. 2015;147:123-135
- Shimaoka M, Xiao T, Liu JH, et al. Structures of the alpha L I domain and its complex with ICAM-1 reveal a shape-shifting pathway for integrin regulation. Cell. 2003;112(1):99-111.
- Kuwano Y, Spelten O, Zhang H, Ley K, Zarbock A. Rolling on E- or P-selectin induces the extended but not high-affinity conformation of LFA-1 in neutrophils. Blood. 2010;116(4):617-624.
- Zarbock A, Lowell CA, Ley K. Spleen tyrosine kinase Syk is necessary for E-selectin-induced alpha(L)beta(2) integrin-mediated rolling on intercellular adhesion molecule-1. Immunity. 2007;26(6):773-783.
- Graham GJ, Handel TM, Proudfoot AEI. Leukocyte adhesion: reconceptualizing chemokine presentation by glycosaminoglycans. Trends Immunol. 2019;40(6):472-481.
- Williams MR, Azcutia V, Newton G, Alcaide P, Luscinskas FW. Emerging mechanisms of neutrophil recruitment across endothelium. Trends Immunol. 2011;32(10):461-469.
- Muller WA. Getting leukocytes to the site of inflammation. Vet Pathol. 2013;50(1):7-22.
- Vestweber D. How leukocytes cross the vascular endothelium. Nat Rev Immunol. 2015;15(11):692-704.
- Woodfin A, Voisin MB, Imhof BA, Dejana E, Engelhardt B, Nourshargh S. Endothelial cell activation leads to neutrophil transmigration as supported by the sequential roles of ICAM-2, JAM-A, and PECAM-1. Blood. 2009;113(24):6246-6257.
- Carman CV. Mechanisms for transcellular diapedesis: probing and pathfinding by ‘invadosome-like protrusions’. J Cell Sci. 2009;122(Pt 17):3025-3035.
- Muller WA. Transendothelial migration: unifying principles from the endothelial perspective. Immunol Rev. 2016;273(1):61-75.
- Mathias JR, Perrin BJ, Liu TX, Kanki J, Look AT, Huttenlocher A. Resolution of inflammation by retrograde chemotaxis of neutrophils in transgenic zebrafish. J Leukoc Biol. 2006;80(6):1281-1288.
- Woodfin A, Voisin MB, Beyrau M, et al. The junctional adhesion molecule JAM-C regulates polarized transendothelial migration of neutrophils in vivo. Nat Immunol. 2011;12(8):761-769.
- Petri B, Sanz M. Neutrophil chemotaxis. Cell and Tissue Research. 2018;371(3):425-436.
- Ward PA. The dark side of C5a in sepsis. Nature Reviews. Immunology. 2004;4(2):133-142.
- Christophe T, Rabiet MJ, Tardif M, Milcent MD, Boulay F. Human complement 5a (C5a) anaphylatoxin receptor (CD88) phosphorylation sites and their specific role in receptor phosphorylation and attenuation of G protein-mediated responses. Desensitization of C5a receptor controls superoxide production but not receptor sequestration in HL-60 cells. J Biol Chem. 2000;275(3):1656-64
- Huber-Lang M, Sarma VJ, Lu KT, et al. Role of C5a in multiorgan failure during sepsis. Journal of Immunology. 2001;166(2):1193-1199.
- Walport MJ. Complement first of two parts. N Engl J Med. 2001;344(14):1058-1066.
- Tisherman SA, Schmicker R, Brasel K, Bulger E, Kerby J, Minei P, et al. Detailed description of all deaths in both the shock and traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium. Ann Surg. 2015;261:586-590.
- Thiessen SE, Van den Berghe G, Vanhorebeek I. Mitochondrial and endoplasmic reticulum dysfunction and related defense mechanisms in critical illness-induced multiple organ failure. Biochim Biophys Acta Mol Basis Dis. 2017;1863:2534-45.
- Hotchkiss RS, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, Matuschak GM, et al. Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Crit Care Med. 1999;27:1230-51.
- Kozlov AV, Duvigneau JC, Miller I, Nürnberger S, Gesslbauer B, Kungl A, et al. Endotoxin causes functional endoplasmic reticulum failure, possibly mediated by mitochondria. Biochim Biophys Acta Mol Basis Dis. 2009;1792:521-30.
- Schiffl H, Fischer R. Five-year outcomes of severe acute kidney injury requiring renal replacement therapy. Nephrol Dial Transplant. 2008;23:2235-41.
- Dias C, Nylandsted J. Plasma membrane integrity in health and disease: significance and therapeutic potential. Cell Discov. 2021;7:4.
- Weidinger A, Müllebner A, Paier-Pourani J, Banerjee A, Miller I, Lauterböck L, et al. Vicious inducible nitric oxide synthase-mitochondrial reactive oxygen species cycle accelerates inflammatory response and causes liver injury in rats. Antioxid Redox Signal. 2015;22:572-86.
- Dungel P, Perlinger M, Weidinger A, Redl H, Kozlov AV. The cytoprotective effect of nitrite is based on the formation of dinitrosyl iron complexes. Free Radic Biol Med. 2015;89:300-10.
- Aisa-Alvarez A, Soto ME, Guarner-Lans V, Camarena-Alejo G, FrancoGranillo J, Martínez-Rodríguez EA, et al. Usefulness of antioxidants as adjuvant therapy for septic shock: a randomized clinical trial. Medicina. 2020;56:619.
- Kitsiouli E, Tenopoulou M, Papadopoulos S, Lekka ME. Phospholipases A2 as biomarkers in ARDS. Biomed J. 2021;44:663-70.
- Bomalaski JS, Steiner MR, Simon PL, Clark MA. IL-1 increases phospholipase A2 activity, expression of phospholipase A2-activating protein, and release of linoleic acid from the murine T helper cell line EL-4. J Immunol. 1992;148:155-60.
- Law RHP, Lukoyanova N, Voskoboinik I, Caradoc-Davies TT, Baran K, Dunstone MA, et al. The structural basis for membrane binding and pore formation by lymphocyte perforin. Nature. 2010:468:447-51.
- Silva CM, Wanderley CWS, Veras FP, Sonego F, Nascimento DC, Gonçalves AV, et al. Gasdermin D inhibition prevents multiple organ dysfunction during sepsis by blocking NET formation. Blood. 2021;138:2702-13.
- Karasu E, Nilsson B, Köhl J, Lambris JD, Huber-Lang M. Corrigendum: Targeting complement pathways in polytrauma- and sepsis-induced multipleorgan dysfunction (Front Immunol. 2019;10:543). Front Immunol. 2019;10:994.
- Kozlov AV, Grillari J. Pathogenesis of multiple organ failure: the impact of systemic damage to plasma membranes. Front Med (Lausanne). 2022;9:806462.