Журнал «Медицина неотложных состояний» Том 17, №4, 2021
Вернуться к номеру
Рідкісний цікавий випадок летальної повітряної емболії після внутрішньовенного контрастування під час комп’ютерної томографії
Авторы: Naved Y. Hasan, Asiah Salem Rugaan
Department of Intensive Care, King Abdullah Medical City, Muzdalifah Road, Al Mashaer, Makkah, Saudi Arabia
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
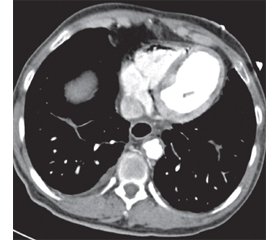
У статті повідомляється про смертельний випадок повітряної емболії. Незважаючи на те що легкі випадки повітряної емболії можуть залишитися непоміченими, це випадок летальної повітряної емболії після внутрішньовенного потрапляння повітря, яка проявилася раптовим початком безімпульсної електричної активності під час комп’ютерної томографії в рентгенологічному відділенні, що вимагало серцево-легеневої реанімації протягом 15 хв. Після повернення спонтанного кровообігу пацієнт був госпіталізований до реанімаційного відділення. Його інтубували та перевели на штучну вентиляцію легенів у шоковому стані. Пацієнт залишався в рефрактерному шоці, незважаючи на підтримуючу терапію. У лабораторії катетеризації знову зареєстровано зупинку серця, і хворого не вдалося реанімувати через 4 год від початкової зупинки серця. Стало відомо, що під час комп’ютерної томографії виявлено значну кількість внутрішньосерцевого повітря, що було ймовірною причиною смерті пацієнта. Цей випадок описує рідкісний стан, що підкреслює важливість ранньої діагностики та нагадує медичному персоналу про необхідність високої настороженості в пацієнтів, які мають фактори ризику та в яких розвивається раптовий шок із гіпоксемією, для вчасного ефективного лікування цього стану, що потенційно загрожує життю.
We are reporting a fatal case of air embolism. Although minor cases of air embolism may go unnoticed, this is a case of fatal air embolism after intravenous entry of air, which presented with sudden onset of pulseless electrical activity during a computed tomography scan in the radiology department, requiring cardiopulmonary resuscitation for 15 min. Subsequently, after admission to the intensive care unit, we achieved return of spontaneous circulation. The patient was intubated and ventilated in a shock state. He remained in refractory shock despite of supportive care. Cardiaс arrest was registered again in the catheterization lab and the patient could not be revived after 4 h from the initial cardiac arrest. А computed tomography scan was reported to reveal a significant amount of intra-cardiac air, which was the likely cause patient’s death. The case is a rare condition, which highlights the importance of early diagnosis and delivers a message to the medical staff to have a high index of suspicion in patients who have risk factors, and who develop sudden shock with hypoxemia, in order to treat this potentially life-threatening condition effectively in a timely manner.
повітряна емболія; безімпульсна електрична активність; серцево-легенева реанімація; шок; смертність
air embolism; pulseless electrical activity; cardiopulmonary resuscitation; shock; mortality
Abbreviations
Introduction
Case Summary
Discussion
/105_2.jpg)
Conclusions
- Ely E. Wesley, MD, MPH, FCCP; Hite R. Duncan MD, FCCP; Baker Albert M., MD, FCCP; Johnson, Margaret M., MD, FCCP; Bowton, David L., MD, FCCM, FCCP; Haponik, Edward F., MD, FCCP. Venous air embolism from central venous catheterization: A need for increased physician awareness. Critical Care Medicine. Oct 1999. Vol. 27(10). 2113-2117.
- Parienti J.J., Mongardon N., Mégarbane B., Mira J.P., Kalfon P., Gros A. et al. Intravascular complications of central venous catheterization by insertion site. N. Engl. J. Med. 2015. 373. 1220–1229.
- Pronovost P.J., Wu A.W., Sexton J.B. Acute decompensation after removing a central line: Practical approaches to increasing safety in the Intensive Care Unit. Ann. Intern. Med. 2004. 140. 1025-1033.
- Mirski M.A., Lele A.V., Fitzsimmons L., Toung T.J. Diagnosis and treatment of vascular air embolism. Anesthesiology. 2007. 106. 164-177.
- Recompression Therapy. In U.S. Navy Diving Manual, Revision 4. Defense department. 1999. 5. 1-50. Available at http://www.coralspringsscuba.com/miscellaneous/usn_manual.htm (Accessed March 3, 2006).
- Niyibizi E., Kembi G.E., Lae C. et al. Delayed hyperbaric oxygen therapy for air emboli after open heart surgery: case report and review of a success story. J. Cardiothorac. Surg. 2016. 11. 167. https://doi.org/10.1186/s13019-016-0553-5.
- Jain K.K. Cerebral Air Embolism. In: Textbook of Hyperbaric Medicine. Gottingen: Hogrefe Publishing, 2009. 103-110.

/104.jpg)
/104_2.jpg)
/105.jpg)