Резюме
Актуальність. Епілепсія є однією з найбільш важливих клінічних проблем, і в той же час це міждисциплінарна проблема. Коморбідні розлади при епілепсії являють собою велику гетерогенну групу різних станів, більшість з яких є психічними розладами (розлад особистості, деменція, депресія, тривожні розлади, психози). Мета дослідження: вивчити супутню патологію епілепсії і непсихотичних психічних розладів у чоловіків молодого віку та особливості її впливу на якість життя пацієнта. Матеріали та методи. У цьому дослідженні були проаналізовані дані нейропсихологічного тестування 40 чоловіків віком 18–44 років. Кореляційний аналіз (коефіцієнт кореляції Пірсона) був використаний для визначення ступеня і характеру взаємозв’язку між досліджуваними параметрами. Усі відмінності і взаємозв’язки, згадані в статті, вважалися статистично вірогідними при р < 0,05. Результати. В усіх пацієнтів у цьому дослідженні були виявлені непсихотичні психічні розлади у формі тривоги, занепокоєння про своє здоров’я і зниження самооцінки. Особиста і ситуативна тривожність у середньому становила 45,60 ± 0,35 бала. Одним iз найбільш поширених непсихотичних розладів у людей з епілепсією є органічний розлад особистості. Аналіз за Міжнародною шкалою вивчення розладів особистості показав, що 32 особи (80 %) мали органічний розлад особистості внаслідок епілепсії. Депресія є найбільш поширеною супутньою патологією, що спостерігається в осіб з епілепсією. Аналіз даних 40 пацієнтів за шкалою Гамільтона для оцінки депресії показав, що легкі депресивні розлади спостерігалися у 18 (45 %) осіб, помірні — у 12 (30 %) і тяжкі депресивні розлади — у 10 (25 %). Глибина проявів депресії корелювала з тривалістю захворювання (r = 0,39; р < 0,05), інтроверсією (r = 0,33; р < 0,05), віком (r = 0,29; р < 0,05) і політерапією (r = 0,53; р < 0,05). Висновки. Таким чином, ми виявили непсихотичні психічні розлади, такі як органічний розлад особистості, деменція, депресія, що характерні для епілепсії в чоловіків молодого віку.
Актуальность. Эпилепсия является одной из наиболее важных клинических проблем, и в то же время это междисциплинарная проблема. Коморбидные расстройства при эпилепсии представляют собой обширную гетерогенную группу различных состояний, большинство из которых являются психическими расстройствами (расстройство личности, деменция, депрессия, тревожные расстройства, психозы). Цель исследования: изучить сопутствующую патологию эпилепсии и непсихотических психических расстройств у мужчин молодого возраста и особенности ее влияния на качество жизни пациента. Материалы и методы. В этом исследовании были проанализированы данные нейропсихологического тестирования 40 мужчин в возрасте 18–44 лет. Корреляционный анализ (коэффициент корреляции Пирсона) был использован для определения степени и характера взаимосвязи между исследуемыми параметрами. Все различия и взаимосвязи, упомянутые в статье, считались статистически достоверными при р < 0,05. Результаты. У всех пациентов в данном исследовании были обнаружены непсихотические психические расстройства в форме тревоги, беспокойства о своем здоровье и снижения самооценки. Личная и ситуативная тревожность в среднем составила 45,60 ± 0,35 балла. Одним из наиболее распространенных непсихотических расстройств у людей с эпилепсией является органическое расстройство личности. Анализ по Международной шкале изучения расстройств личности показал, что у 32 человек (80 %) было органическое расстройство личности вследствие эпилепсии. Депрессия является наиболее распространенной сопутствующей патологией, наблюдаемой у лиц с эпилепсией. Анализ данных 40 пациентов по шкале Гамильтона для оценки депрессии показал, что легкие депрессивные расстройства наблюдались у 18 (45 %) человек, умеренные — у 12 (30 %) и тяжелые депрессивные расстройства — у 10 (25 %). Глубина проявлений депрессии коррелировала с длительностью заболевания (r = 0,39; р < 0,05), интроверсией (r = 0,33; р < 0,05), возрастом (r = 0,29; р < 0,05) и политерапией (r = 0,53; р < 0,05). Выводы. Таким образом, мы выявили непсихотические психические расстройства, такие как органическое расстройство личности, деменция, депрессия, которые характерны для эпилепсии у мужчин молодого возраста.
Background. Epilepsy is one of the most important clinical problems and at the same time it is an interdisciplinary challenge. Comorbid disorders in epilepsy represent an extensive heterogeneous group of various conditions, most of which are mental disorders (personality disorder, dementia, depression, anxiety disorders, psychoses). The objective is to study the comorbidity of epilepsy and non-psychotic mental disorders in young men and the characteristics of its impact on the quality of life of a patient. Materials and methods. This study analyzed data from neuropsychological testing of 40 men aged 18–44 years. The correlation analysis (Pearson correlation coefficient) was used to determine the degree and nature of the relationship between the study parameters. All the differences and relationships mentioned in the article were considered statistically valid at p < 0.05. Results. All patients in this study were found to have non-psychotic mental disorders in the form of anxiety, concern about their health, and a decrease in self-esteem. Personal and situational anxiety averaged 45.60 ± 0.35 points. One of the most common non-psychotic disorders in individuals with epilepsy is organic personality disorder. Analysis on the International Personality Disorder Examination scale showed that 32 people (80 %) had organic personality disorder due to epilepsy. The depression is the most common comorbidity observed in individuals with epilepsy. An analysis of the data of 40 people using Hamilton Depression Rating Scale showed that mild depressive disorders were observed in 18 (45 %) people, moderate — in 12 (30 %), and severe depressive disorders — in 10 patients (25 %). The depth of manifestations of depression correlated with the duration of the disease (r = 0.39; p < 0.05), introversion (r = 0.33; p < 0.05), age (r = 0.29; p < 0.05) and polytherapy (r = 0.53; p < 0.05). Conclusions. Thus, we have identified non-psychotic mental disorders such as organic personality disorder, dementia, depression, which are typical for epilepsy in young men.
Introduction
Epilepsy is the third most common pathology among all organic diseases of the brain. According to the World Health Organization (WHO), around 65 million people worldwide suffer from epilepsy. Annually, 2.5 million new cases of epilepsy are recorded.
The prevalence of this pathology in developed countries is 5–10 cases per 1,000 population. According to the results of demographic studies conducted in developed countries, the incidence of epilepsy ranges from 0.28 to 0.53 per 1,000 population. The prevalence of this disease ranges from 0.96 to 10 cases per 1,000 population in the Commonwealth of Independent States. The prevalence of epilepsy ranges from 50 to 73 cases per 100,000 population in various regions of Ukraine (an average of 73.9 per 100,000). In addition, the average incidence in men (53.7 per 100,000) is slightly higher than in women (46.3 per 100,000) [13].
Epilepsy is one of the most important clinical problems and at the same time it is an interdisciplinary challenge that is directly related to psychiatry, neurosurgery, medical psychology and neurophysiology.
This disease has a significant negative effect on all spheres of the patient’s life, reducing its quality. The quality of life (QOL) in people with epilepsy, especially patients of young age, involves a socially active lifestyle [2].
In everyday life, men with epilepsy regularly experience difficulties. Basically, this is a decrease in social and personal ambitions, low self-esteem compared with healthy people, an increase in the level of anxiety and depression. Depression in people with epilepsy is often manifested itself by symptoms that can be considered as side effects of antiepileptic drugs, as well as manifestations of epilepsy per se (sleep disturbances, changes in appetite, behavioral disorders, inhibition or excessive irritability, etc.).
Comorbid disorders in epilepsy represent an extensive heterogeneous group of various conditions, most of which are mental illnesses (personality disorder, dementia, depression, anxiety disorders, psychoses).
Affective, anxiety disorders, psychosis, attention deficit hyperactivity disorder, and autism spectrum disorders are often diagnosed with epilepsy as comorbid conditions. A number of specialists [11, 12] consider mental and behavioral disorders to be complications of epilepsy, and other scientists [3, 4, 7, 13] demonstrated a two-way orientation of the causal relationship between them.
The purpose is to study the comorbidity of epilepsy and non-psychotic mental disorders in young men and to investigate the characteristics of the impact of this disease on the quality of life of a patient.
Materials and methods
This study involved 40 men aged 18–44 years. According to the WHO classification, all subjects belonged to a group of young people. The average age of the patients was 33.90 ± 2.12 years.
Men with significant somatic pathology, acute and chronic, as well as brain tumors, acute craniocerebral injuries and acute infectious diseases of various etiologies were not enrolled.
The study included neuropsychological testing using the Quality of Life in Epilepsy-31 Inventory (QOLIE-31), the Mini-Mental State Examination (MMSE), and the International Personality Disorder Examination (IPDE) based on the Diagnostic and Statistical Manual of Mental Disorders-5, State-Trait Anxiety Inventory (STAI), Clinical Dementia Rating (CDR) scale (Morris J.C., 1993), Hamilton Depression Rating Scale (HDRS). Electroencephalography (EEG), EEG-video monitoring were used as screening methods.
The general examination and determination of the basic physical data to exclude the actual somatic patho-logy, as well as a neurological examination were carried out according to conventional methods.
We analyzed the QOL of patients with epilepsy, the nature of epileptic seizures, their frequency, duration, and also took into account other complaints, anamnestic data, and a family history to identify the genetic predisposition to epilepsy. The form of epilepsy and the type of epileptic seizures were determined according to the International Classification of Epilepsy and Epileptic Seizures (International League Against Epilepsy, 2017).
The correlation analysis (Pearson correlation coefficient) was used to determine the degree and nature of the relationship between the study parameters. All the differences and relationships mentioned in the article were considered statistically valid at p < 0.05.
Results and discussion
Analysis of the data from 40 patients (100 %) on the QOLIE-31 showed that 6 people (15 %) rated their QOL as very low. Low and average QOL scores were obtained from 10 (25 %) and 16 (40 %) patients, respectively. In 8 (20 %) individuals, the parameters were within the range of good QOL (Fig. 1). Evaluation of the high quality of life has not been received.
According to the International Classification of Epilepsy and Epileptic Seizures, all men were divided depending on the form of epilepsy. The data are shown in Fig. 2.
As it can be seen from the above data, combined focal and generalized epilepsy prevailed in young men.
According to the etiology, structural epilepsy was detected in 21 people (52.5 %), infectious epilepsy — in 11 (27.5 %) and epilepsy of unknown etiology — in 8 (20 %). The duration of the disease (M ± SD) averaged 12.6 ± 4.3 years.
In this group of patients, epileptic seizures with focal onset dominated, which may be associated with the prevalence of local structural brain lesions (Fig. 3). The seizures with generalized onset had a significantly smaller proportion.
Despite adequate antiepileptic treatment, frequent and moderate seizures were predominant in the examined patients (45 and 25 %, respectively), and only 30 % had rare seizures (Fig. 4). Thus, long-term (on average 12.6 ± 4.3 years) drug-resistant epilepsy prevailed in this group.
All patients in this study were found to have non-psychotic mental disorders in the form of anxiety, concern about their health, and a decrease in self-esteem. Personal and situational anxiety was assessed using the STAI, the score averaged 45.60 ± 0.35 points. Thus, the majority of men were highly anxious individuals, prone to perceive a threat to their self-esteem and life activi-ty in a wide range of situations and respond with a very pronounced state of anxiety.
/64.jpg)
One of the most common non-psychotic disorders in individuals with epilepsy is organic personality disorder. In the formation of changes, a certain role belongs to the individuals’ reactions to the attitude of others, as well as to the awareness of their disease and related defects [1]. S. Waxman and N. Geschwind [10] identified such signs of altered behavior in epilepsy as increased emotions, thoroughness, increased religiosity, decreased sexual activity and hypergraphia. The authors designated this condition as interictal behavior syndrome, which was later referred to as Gastaut-Geschwind syndrome in psychiatric literature. Analysis on the IPDE scale showed that 32 people (80 %) had an organic personality disorder due to epilepsy.
The diffuse changes in bioelectric brain activity were detected with the reduction of high-amplitude slow fluctuations and signs of cerebral cortex irritation in the form of the appearance of multiple sharp waves, peaks, genera-lized synchronous bursts consisting of pointed waves on the EEG in patients with personality changes. The dominant rhythms were: alpha with delta — 3 %, theta — 1 %, alpha — 52 %, beta-1 — 39 %, beta-2 — 1 %. More often paroxysmal activity was recorded in the left temporal region, less often — in the right temporal region. In most patients, generalized bursts of paroxysmal activity were reported, indicating involvement of the brain stem in the pathological process.
It can be assumed that a long and often incurable course of epilepsy, the presence of interictal epileptiform activity and structural damage to the brain lead to a gradual disorganization of the intellectual-mnestic, emotional-volitional and behavioral spheres in young men with epilepsy.
The cognitive impairment is often a clinical manifestation of epilepsy. Various factors play an important role in the pathogenesis of cognitive impairment: the etio-logy of the disease, the type and frequency of epileptic seizures, interictal epileptiform activity on the EEG, premorbid factors, the intake of certain antiepileptic drugs, psychosocial factors that lead to aggravation of seizures [9].
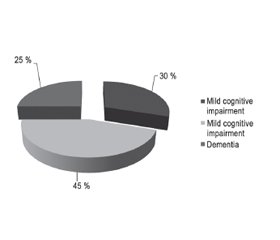
The MMSE was used in this study [6]. Analysis of the test data in 40 patients (100 %) showed that 12 (30 %) of them had mild cognitive impairment. Moderate cognitive impairment was observed in 18 (45 %), dementia — in 10 (25 %) people (Fig. 5).
The moderate cognitive impairment and dementia were most common in patients with combined focal and generalized epilepsy, and people with focal and undisclosed form of epilepsy were more likely to experience mild cognitive impairment. Unilateral, mainly temporal, foci of activity on the EEG with different localization in the brain were typical for individuals with mild cognitive disorders. The dominant rhythms were: alpha with delta — 10 %, theta — 14 %, alpha — 32 %, beta-1 — 24 %, beta-2 — 20 %. The EEG of patients with moderate cognitive disorders was characterized by disorganization, hypersynchronization of electrical activity, and increased slow wave activity. The dominant rhythms were: theta with delta — 26 %, theta — 32 %, alpha — 18 %, beta-1 — 14 %, beta-2 — 10 %. Cognitive impairment correlates with a decrease in fast wave activity in the frontal and parietal regions of the brain (r = 0.45; p < 0.05). At the same time, memory is disrupted, as frontal and parietal areas are involved in passive processes of storing and recalling information.
The CDR scale was used to determine the severity of dementia (Morris J.C., 1993). Data analysis found that 6 people had a questionable stage (CDR-0.5) and 4 men — a mild stage (CDR-1).
Constant mild forgetfulness, incomplete reproduction of events are typical for patients with questionable dementia (CDR-0.5). The person is fully oriented, except for slight difficulties with orientation in time. Such people have minor violations in the field of social activity. The patients are completely self-caring.
Individuals with mild dementia (CDR-1) experienced moderate memory decline (especially on current events) affecting daily activity. The patients had moderate time orientation disorder, moderate difficulties with solving problems, and required to be encouraged to act at this stage of dementia.
The EEG recorded activity with sharp peaks in the form of single waves, as well as “sharp wave — slow wave”, “spike-and-wave” or “polyspike-and-wave” complexes. The spatial distribution of these waves was different. Bilaterally synchronous paroxysmal activity is also indicative of dementia. The ratio of rhythms on the EEG was as follows: delta — 24 %, theta — 27 %, alpha — 14 %, beta-1 — 19 %, beta-2 — 16 %.
The depression is the most common comorbid disorder observed in individuals with epilepsy. These patients face many psychosocial problems during their life [7]. The action of anticonvulsants, as well as the neurobio-logy of epilepsy itself significantly influences the etiology of depression in individuals with epilepsy. Such patients have a significantly increased risk of suicidal thoughts and ideations. Reduced quality of life also leads to mood disorders and, as a result, to depression.
An analysis of the data of 40 people using the HDRS showed that mild depressive disorders were observed in 18 (45 %) people, moderate — in 12 (30 %), and severe depressive disorders — in 10 (25 %) patients (Fig. 6).
/65.jpg)
There was a tendency to desynchronization, an increase in the beta activity (15–20 Hz) mainly in the frontocentral and parietal leads, more often on the right on the EEG. The dominant rhythms were: beta with components of delta — 12 %, theta — 14 %, alpha — 17 %, beta-1 — 39 %, beta-2 — 18 %. Patients with depression showed a decrease in intra- and interhemispheric cohe-rence, as well as a decrease in intrahemispheric integration of bioelectric processes in the theta range (4–8 Hz) in the right temporal regions and in the beta range in the posterior temporal regions (13–17 Hz). Also, during EEG-video monitoring in patients with depression, sleep disturbances are observed. At the neurophysiological level, the symptoms of sleep disturbances in depression in the form of difficulty falling asleep and frequent awa-kenings correspond to a decrease in the duration of the slow wave sleep, in the latent period of the onset of the rapid eye movement sleep and an increase in its overall duration, pathology of the sleep microarchitecture in the form of a greater representation of beta and alpha waves and a decrease in delta activity, the appearance of right hemispheric asymmetry of slow and fast rhythms during the fast microwave phase. The depth of manifestations of depression correlated with the duration of the disease (r = 0.39; p < 0.05), introversion (r = 0.33; p < 0.05), and age (r = 0.29; p < 0.05) and polytherapy (r = 0.53; p < 0.05).
Conclusions
1. This study indicates the diversity of non-psychotic mental disorders associated with epilepsy. Often, comorbid conditions progress and their effect on the health and quality of life of the patient become more significant compared to epilepsy.
2. It has been established that with an increase in the duration of the disease in young men with focal seizures, negative emotional and personality components of the attitude to the disease significantly increase in the form of neurasthenic, melancholic, apathetic and egocentric manifestations. Most men had an organic personality disorder. Mild-to-moderate cognitive impairment, as well as dementia were also observed. Cognitive decline correlates with a decrease in the presence of fast wave activity in the frontal and parietal regions of the brain (r = 0.45; p < 0.05).
3. The mild depressive disorders prevailed in young men. The depth of depression manifestations correlated with the duration of the disease(r = 0.39; p < 0.05), introversion (r = 0.33; p < 0.05), age (r = 0.29; p < 0.05), and polytherapy (r = 0.53; p < 0.05).
4. The quality of life of patients with epilepsy is significantly reduced. The perception of the quality of their life is more dependent on emotional well-being, cognitive and social functioning. The most significant factors that determine low quality of life indicators are the duration of epilepsy, frequency of seizures, and depression.
5. The epileptiform changes in bioelectric activity during the interparoxysmal period (mainly in the frontocentral and parietal regions) can lead to a damage to neuronal networks and, accordingly, be one of the components of the formation of psychoemotional and cognitive disorders.
Thus, we have identified non-psychotic mental disorders such as organic personality disorder, dementia, depression, which are typical for epilepsy in young men.
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Список литературы
1. Austin J.K., Harezlak J., Dunn D.W., Huster G.A. Behavior problems in children before first recognized seizures. Pediatrics. 2001. 107. 96-102.
2. Baker G. Quality of life of people with epilepsy: a European study. Epilepsia. 1997. 38(3). 353-362.
3. Barragan E., Cruz E., Urrutia M. Prevalence of attention deficit disorder in paediatric epilepsy patients. Epilepsia. 2006. 47(4). 179.
4. Barragan E., Cruz E., Urrutia M. Neurocognitive differences between frontal and temporal seizures in pediatric epilepsy. Epilepsia. 2006. 47(4). 206.
5. Broicher S.D., Kuchukhidze G., Grunwald T., Krämer G., Kurthen M., Jokeit H. “Tell me how do I feel” — emotion recognition and theory of mind in symptomatic mesial temporal lobe epilepsy. Neuropsychologia. 2012. 50(1). 118-128.
6. Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975. 12(3). 189-198.
7. Gaitatzis A., Trimble M.R., Sander J.W. The psychiatric comorbidity of epilepsy. Acta Neurol. Scand. 2004. 110. 207-220.
8. Kanner A.M. Depression in epilepsy: prevalence, clinical semio-logy, pathogenic mechanisms, and treatment. Biol. Psychiatry. 2003. 54. 388-398.
9. Lodhi S., Agrawal N. Neurocognitive problems in epilepsy. Advances in Psychiatric Treatment. 2012. 18. 232-240.
10. Waxman S.G., Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch. Gen. Psychiatry. 1975. 32. 1580-1586.
11. Глухова Л.Ю. Аутистический эпилептиформный регресс. Вест. эпилептол. 2012. 1. 3-11.
12. Евтушенко С.К. Разрушительные и труднокурабельные формы эпилепсии и эпилептические энцефалопатии. Междунар. неврол. журн. 2012. 6(52). 16-21.
13. Марценковський І.А. Протиепілептичні препарати та інші засоби лікування епілепсій з розладами спектра аутизму. Укр. вісн. психоневрол. 2014. 3(80). 121-126.
14. Марценковский И.А., Марценковская И.И. Эпилепсия и коморбидные расстройства психики и поведения. Укр. мед. часопис. 2015. 4(108). 43-53.
15. Мищенко Т.С. Деменция — это не нозологическая форма, а синдром. Neuronews: Психоневрология и нейропсихиатрия. 2009. 2(1). 6-9.
16. Electronic source: http://www.moz.gov.ua
/63.jpg)
/64.jpg)
/65.jpg)