The article was published on p. 158-162
Itsenko — Cushing disease (hypercorticoidism) brings together a large group of signs and progressive symptoms wich reflect the prolonged and excessive influence of glucocorticoids on the tissue. European population studies reported about 2–3 cases per 1 million inhabitants a year. The frequency of new cases of pituitary Cushing’s syndrome in the USA ranges from 0,7 to 2,4 cases per 1 million persons per year, that is from 200 to 700 new cases annually. In 90 % of cases of pituitary Cushing’s syndrome the source of corticotropin is pituitary microadenoma, in 5–7 % — macroadenoma, in other cases it is cell hyperplasia [6, 27].
The syndrome of endogenous hypercorticism was first described in 1912 by American physician Harvey Cushing, and in 1924, irrespective of him, by Odessa neurologist N.M. Itsenko [7].
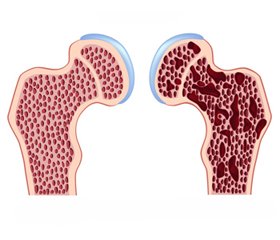
Steroid osteoporosis that develops as a result of pathologic effect on bone of the excessive amount of endogenous glucocorticosteroids (GCS), appears in 95 %, and fractures of the spine — in 40 % of patients [3]. Osteoporosis causes a significant functional limitation of mobility of patients and in some cases — disability, and therefore is considered as one of the most important complications of this disease [16, 26].
Symptoms of endogenous hypercorticism are very specific and varied [1, 18]. At the study of patients with Itsenko — Cushing disease most frequently can be detected following clinical symptoms and syndromes: overweight (94 %), hypertension (60–94 %), systemic osteoporosis (30–80 %), impaired sexual function (85 %) trophic changes of the skin (stretch marks, dryness, acne and pustular lesions) and hypertrichosis (30–77 %), myopathy (75 %), defective carbohydrate metabolism/diabetes mellitus (30–70 %), infectious complications (20–70 %), nephrolithiasis/urolithic illness (30 %) [6, 10]. A variety of clinical manifestations of Itsenko — Cushing disease complicates a timely diagnosis of it. According to the European Registry of patients with Cushing’s syndrome (ERCUSYN) the median of the diagnosis delay is 2 years [33]. A poor prognosis of Itsenko — Cushing disease is caused by involving to pathological process the major systems and organs, with the development of cardiovascular, cerebrovascular and infectious complications [24, 28, 29]. According to R. Feelders et al. [27], even amid remission, patients quali–ty of life is greatly reduced. Progression of the disease leads to disability and reduce life expectancy. The risk of death in case of Itsenko — Cushing disease is in 2 times higher than that in the general population [30]. In the natural course of the disease (without treatment), 5-year survival rate is 50 %. According O. Dekkers et al. [31, 32], increased mortality of patients with Itsenko — Cushing disease is associated with the duration of excessive production of cortisol.
In children and adolescents early symptoms of hypercorticism are growth decelerates, due to the reduction or termination of synthesis of growth hormone, and delay skeletal differentiation; there is a difference between the passport and the bone age in 1–5 years. Steroid osteoporosis with bone demineralization and inhibition of protein matrix synthesis in any age refers to the most serious manifestations of hypercorticism. Expression of the process depends on the degree and duration of hypercorticism.
Glucocorticoid hormones have a direct and indirect influence on the development of bone structures. In direct action we understand the direct effect on cells of the skeletal system — osteoblasts and osteoclasts. The impact of GCS on bone formation can be divided into two phases: the fast and the slow one. The fast phase is associated with progressive bone resorption, and the slow — with continued negative effect on bone formation.
GCS reduce the number of osteoclasts in bone tissue and decrease their functional activity. GCS suppress the replication activity of cells-predecessors of osteoblasts, reducing the pool of cells that later could be differentiated into osteoblasts. In the presence of excess of GCS, cells-predecessors terminate their differentiation or turn later in adipocytes. Moreover, steroids have a negative effect on the already functional activity of mature cells. GCS suppress the synthesis by osteoblasts of the first type of collagen, the main substance of the extracellular bone matrix, thus reducing the amount of matrix for further mineralization. Steroid hormones stimulate apoptosis of osteoblasts and osteocytes, activating caspase‑3. Thus, all of the above leads to a decreased number of osteoblasts and reduced bone formation.
GCS influence on osteoblasts. Under the action of hormones, increases the production of IL‑6, which has a positive effect on the function of osteoclasts, and reduces production of interferon-beta, which has an opposite effect, besides steroids increase lifespan of osteoclasts and reduce their apoptosis.
GCS decrease the expression of IGF‑1, which increases synthesis of the first type of collagen, reduce its degradation and activate apoptosis of osteoblasts [23].
Steroid hormones have an indirect influence on bone formation, as they are antagonists of vitamin D, inhibiting calcium absorption in the gastrointestinal tract and reducing the expression of specific calcium channels in the duodenum. GCS cause in intestinal cells disintegration of 1,25 (OH) 2-D3 (1,25-dihydroxyvitamin D3, calcitriol) to inactive metabolites which cannot be absorbed due to lack of sensitivity of the intestinal epithelial cells to them.
Influence of GCS on renal tubules is similar with its effect on enterocytes, that there is increased loss of calcium in the urine by ion diffusion. GCS have catabolic effects on skeletal muscle, this, in turn, reduces bone mineralization and increases the risk of osteoporosis according to mechanostatic theory [2, 20].
Diagnosis. In childhood steroid osteoporosis has a long asymptomatic course and usually manifests by growth retardation. In addition to the retardation may also be reduction of achieved growth caused by vertebral deformities and decline of their height. Loss of bone mass and deformation of vertebral bodies are unnoticed for a long time. The first symptom may be chest pain, which is caused by small fractures of the ribs. With the development of aseptic necrosis of the head of femoral bone, patients gets a disturbed walking — it is «like a duck» [12].
For the diagnosis of osteoporosis, caused by excessive intake of GCS, is enough to make X-ray of wrist or ankle joints, pelvic bones, spine and skull. In this case takes into account change of the ratio between the diameter and thickness of bone, expansion of spinal canal, increasing of bone transparency, thinning of bone trabecula and locking plates of glenoid cavity. The degree of severity varies from a mild bone osteoporosis to the disappearance of bone structure. In vertebral bodies can be find increased contrast of locking plates and vertical striations due to thickening of remaining trabeculas. Maybe also change the height of vertebral bodies due to their reduction and compression fractures. At the steroid osteoporosis on X-ray also occur granular foci of enlightenment in bones of the skull and hands. Downside of plain radiography is that the first changes become visible at the loss of 30–40 % of bone material, which reduces the value of this method for early diagnosis. Furthermore, this method, on its accuracy and reproducibility of the results, is significantly inferior to modern methods of osteodensitometry [11, 15].
Photonic and X-ray densitometers are divided into mono- and dichromatic. Monochromatic make it possible to explore only cortical tissue and dichromatic methods — cortical and trabecular bones, which allows to determine bone mineral density of the peripheral and axial skeleton [17, 19].
Since 1994, on the recommendation of the WHO experts the gold standard for diagnosis of osteoporosis consider Dual Energy X-Ray Absorbciometry (DXA or DEXA), which combines the ability to study axial and peripheral areas of the skeleton, high sensitivity and specificity, accuracy and low error of reproducibility, the minimum dose and speed of study. Many devices are equipped with «total body» program, that allows to determine the content of minerals throughout the skeleton, explore soft tissue (muscle and fat). The DXA method as a result of scan a certain areas of the skeleton is measured on two values: area of scanning surface (Area, cm2) and bone mineral content (BMC, g), with further calculation of one clinically significant parameter — projection bone mineral density (BMD) (BMD = BMC/Area, g/cm2). Since osteoporosis is not the same in different parts of the skeleton, it is necessary to use standard scanning program (research of standard body parts in standard position) for the lumbar, distal forearm, hip, and so on. Currently, the most widely used standard automatic software for evaluation of mineral density of the lumbar spine (in two projections) of the proximal femur, forearm and total body. Computer software of osteodensitomerty contains the reference framework — normative indicators by gender and age. A special importance for researches in pediatric practice has the presence of a special pediatric program that allows to define DXA in children from the birth. DXA data is automatically compared with the standard, is calculated deviations of individual values from medieval norms (Z criterion), from peak bone mass in persons of corresponding sex (T-test) and determined the value of the standard deviation of the average indicators. The value of the standard deviation allows to quantitatively distinguish variants of the norm, osteopenia and osteoprosis [13, 23]. In pediatric, in contrast to adults, the diagnostic value has only Z criterion. This indicator depends on age. It is considered that the most informative is study of two areas of the skeleton, as it reduces probability of errors and the risk to «miss» the osteoporosis. The question of the study of the central or peripheral skeleton depends of the clinical task. It is believed that DXA measurement gives an answer to key clinical questions: what is the risk of fractures and how changes bone density with patients aging or during the therapy [11].
The development of quantitative computer tomography method allows spatial separation of cortical and trabecular bones and get volume instead of planar characteristics of it. In addition, computer tomography excludes the projection imposition of adjacent bone structures and surrounding tissue, what increases the accuracy of measurement of bone mass. However, this method is expensive and gives a few more radiation exposure, which limits its use in pediatric patients [4].
In recent years is developing quantitative ultrasound densitometry that allows to evaluate bone status by speed of passage of the ultrasonic waves through the bone (SOS — Speed Of Sound) and the magnitude of its attenuation in bone (BUA — Broadband Ultrasound Attenuation). Named figures reflect the elasticity, hardness and strength of bone. However, the comparative evaluation of ultrasound and X-ray densitometry gives a conflicting results. It is believed that both methods are able to accurately assess bone mass and risk of fracture [14, 22, 25]. According to other researchers, ultrasound densitometry opportunities are limited. However, there are many supporters of this method. They believe that quantitative ultrasound is promising. There have been its simplicity and convenience for screening. The positive qualities of ultrasound densitometry includes the absence of radial load, speed of the research, greater accuracy, good reproducibility and portability of the method, that can be used in pediatric patients, including for population studies [9, 20, 22].
By eploying the methods of «bone densitometry» can be evaluated the basic parameters of bone strength, but these methods do not give any information about the level of bone metabolism.
Bone markers are the predictors of bone loss, skeletal bones fractures and can be used for monitoring of antiosteoporosis therapy. Its proved that biochemical markers allows on early stage to diagnose signs of bone loss and thereby to predict risk of fractures; it was discovered informative of markers to assess the effectiveness of various methods of osteoporosis prevention. By this biochemical indices can be evaluated the effectiveness of therapy, the adequacy of dosage and its tolerability [5, 8, 21]. Especially productive are bone markers for assessing the effectiveness of therapy in a comparatively short period of time when densitometric studies are not informative yet (believe that repeated densitometric studies need to perform no more frequently than once a year). The combination of densitometry studies and biochemical markers of bone metabolism allows to receive more information about the risk of osteoporosis. To assess the effectiveness of the therapy is recommended to examine biochemical markers every three months after starting treatment. In the study of biochemical markers is necessary to take into account factors that affect the reproducibility of results: diet, storage conditions of the material, biological factors (circadian and seasonal fluctuations, menstrual cycle, age, gender, presence of comorbidities, etc.). It was found the interrelation between biochemical markers of bone metabolism with bone mineral density and linear growth.
Among the biochemical markers of bone metabolism were distinguished:
— markers of bone formation, osteocalcin (defined in serum or plasma); isoenzyme of alkaline phosphatase — bone alkaline phosphatase (defined in serum or plasma); C- and N-terminal propeptide procollagen type 1 (determined in serum);
— markers of bone resorption, tartrate-resistant acid phosphatase (determined in serum); products of degradation of collagen type 1 — cross-connections, pirydynolin and deoxypirydynolin in urine, structurally closely related so-called cross-linking C- and M-terminal telopeptides of collagen type 1 (determined in serum or plasma, and in urine); hydroxyprolin in urine — a product of collagen de–gradation (determined in urine).
Osteocalcin (OC) is synthesized by osteoblasts and is the most common noncollagen protein of bone matrix that is specific to bone and dentin. OC is considered as one of the most informative biochemical markers of bone formation and speed of «bone turnover». The function of osteocalcin is not fully understood, but found that the chemical structure allows it to interact with hydroxyapatite. In ontogenesis OС appears simultaneously with the start of bone mineralization. OС includes in the extracellular matrix of bone tissue. It was shown that it appears in blood as a result of secretion from bone cells, and not the breakdown of bone matrix. OC level in serum correlates with the formation of bones that has been proved via histomorphometry and study of kinetics of calcium metabolism. OS level increases with age, rising slightly at the age of 5–6 years and reaches its maximum for girls of 11–12 years old, boys — of 13–14 years, which corresponds to the maximum rate of body length at this age. After the growth jump its rate decreases. There is evidence that girls reach adult values of OS earlier than boys. The content of OS in children is more related with the speed of growth than the biological age.
It was established that during the growth bone alkaline phosphatase (BAP) is slightly increased in 5–6 years old children and reaches its peak in 11–12 years for girls, for boys — up to 13–14 years. Its level is reduced in late puberty and till 12 years girls have BAP level slightly higher than boys, and then it drops sharply, which is probably due to the growth of estrogen on the background of puberty and reduced bone formation activity.
Estimation of BAP dynamics is important to characterize bone mineral density. A direct correlation dependence between the BAP activity and ionized blood calcium, that is coordinated with the data on participation of BAP in mineralization of bone matrix. There is evidence that the level of BAP in girls at puberty is in 10 times higher than in women of reproductive age.
Osteoclasts secrete a mixture of acid and neutral proteases, which digest collagen fibers sequentially and in bloodstream gets molecular fragments containing pirydynolin. Original fragments, produced by osteoclasts are further splitting in the liver and kidneys to low molecular weight compounds and excreted by the urine. Carboxy Terminal (C-terminal telopeptides) of human collagen type 1 are the most informative markers of bone resorption. Since collagen forms the basis of the organic matrix of bone, the content of telopeptide in the serum and urine can accurately describe the process of bone resorption. It was established that telopeptide concentration tends to increase with the age of the child. There have been a relative increase of
C-terminal telopeptide during the growth jump (5–6 years) and a significant rise during puberty. During puberty are observed two peaks of rise of biochemical markers in serum. The first corresponds to the age of 11–12 years and is associated with the highest rate of growth of the skeleton in girls, the second — 13–14 years and is caused by an increase of body length in boys. Received data showed a high rate of remodeling that is a metabolic state of the organism, when intensive are both processes formation and bone resorption.
Despite the recent scientific advances in early diagnosis of osteoporosis in Ukraine, especially in pediatric patients, this question, unfortunately, is still problematic, which is primarily due of the lack in pediatric health care facilities of densitometers, equipped with special programs for estimation of children’s bone density; national standards; laboratory equipment and reagents for the determination of markers of bone metabolism.
Список литературы
1. Автоматизированный электрохемилюминесцентный метод определения кортизола в слюне для диагностики эндогенного гиперкортицизма среди пациентов с ожирением / Ж.Е. Белая, А.В. Ильин, Г.А. Мельниченко и др. // Ожирение и метаболизм. — 2011. — № 2. — С. 56-63. — doi: 10.14341/2071-8713-4954.
2. Актуальные проблемы остеопороза / Под ред. В.И. Струкова. — Типография «Ростра», 2009. — С. 342.
3. Бухман А.И. Основные принципы рентгенодиагностики и дифференциальной рентгенодиагностики остеопороза / А.И. Бухман // Международный медицинский журнал. — 1999. — Т. 2, № 3–4. — С. 213-217.
4. Власова И.С. Современные методы лучевой диагностики остеопороза / И.С. Власова // Вестник рентгенологии и радиологии. — 2002. — № 1. — С. 37-42.
5. Возрастные особенности изменений биохимических маркеров костного ремоделирования у детей / А.А. Баранов, Л.А. Щеплягина, М.И. Баканов и др. // Рос. педиатр. журн. — 2002. — № 3. — С. 7-12.
6. Дедов И.И. Болезнь Иценко-Кушинга: клиника, диагностика, лечение: Практическое руководство для врачей / Под ред. И.И. Дедова, Г.А. Мельниченко. — М., 2012. — С. 12-14.
7. Дедов И.И. Эндокринология: Нац. руководство / И.И. Дедов, Г.А. Мельниченко (ред.). — М.: Гэотар-Медиа, 2009. — С. 95-97.
8. Ермакова И.П. Сывороточные биохимические маркеры в диагностике остеопороза / И.П. Ермакова, И.А. Пронченко // Остеопороз и остеопатии. — 1998. — № 1. — С. 24-26.
9. Кудрявцев П.С. Методы и аппаратура для ультразвуковой денситометрии / П.С. Кудрявцев // Остеопороз и остеопатии. — 1999. — № 2. — С. 44-47.
10. Метаболические осложнения эндогенного гиперкортицизма. Выбор пациентов для скрининга / Ж.Е. Белая, Л.Я. Рожинская, Н.В. Драгунова и др. // Ожирение и метаболизм. — 2013. — № 1. — С. 26-31. — doi: 10.14341/2071-8713-5068.
11. Остеопения у детей: диагностика, профилактика и коррекция: Пособие для врачей / Л.А. Щеплягина, Т.Ю. Моисеева, М.В. Коваленко и др. — М., 2005. — 23 с.
12. Остеопороз: эпидемиология, клиника, диагностика, профилактика и лечение / АМН Украины; под ред. Н.А. Коржа, В.В. Поворознюка, Н.В. Дедух, И.А. Зупанца. — Х.: Золотые страницы, 2002. — 648 с.
13. Поворознюк В.В. Захворювання кістково-м’язової системи в людей різного віку (вибрані лекції, огляди, статті) / В.В. Поворознюк. — К., 2004. — Т. 2. — 480 с.
14. Поворознюк В.В. Структурно-функціональний стан кісткової тканини у дітей та підлітків України: дані ультразвукової денситометрії / В.В. Поворознюк // ПАГ. — 1999. — № 4. — С. 154.
15. Рахманов А.С. Костная денситометрия в диагностике остеопении / А.С. Рахманов, А.В. Бакулин // Остеопороз и остеопатии. — 1998. — № 1. — С. 43-45.
16. Рожинская Л.Я. Минеральная плотность ткани при эндогенном и экзогенном гиперкортицизме / Л.Я. Рожинская // Остеопороз и остеопатии. — 2000. — № 2. — С. 12-17.
17. Сміян І.С. Вторинний остеопороз у дитячому віці та перший досвід використання двофотонної денситометрії в Україні для його діагностики / І.С. Сміян // ПАГ. — 1999. — № 4. — С. 154.
18. Современный взгляд на скрининг и диагностику эндогенного гиперкортицизма / Ж.Е. Белая, Л.Я. Рожинская, Г.А. Мельниченко, И.И. Дедов // Проблемы эндокринологии. — 2012. — Т. 58, № 4. — С. 35-41. — doi: 10.14341/probl201258435-41.
19. Состояние костной ткани у детей и подростков по данным однофотонной денситометрии / Н.В. Дедух, Н.С. Шевченко, С.Д. Шевченко и др. // Ортопедия, травматология и протезирование. — 1999. — № 1. — С. 13-16.
20. Фролова Т.В. Оцінка структурно-функціонального стану кісткової тканини дітей шкільного віку та підлітків за результатами ультразвукової денситометрії: Метод. рекомендації / Т.В. Фролова, М.О. Корж, С.П. Шкляр. — Харків, 2006. — 26 с.
21. Цветная И.Н. Возрастные особенности концентрации С-концевых телопептидов в плазме крови у детей 1–6 лет / И.Н. Цветная, Н.П. Ершова // Поликлиника. — 2006. — № 1. — С. 52-55.
22. Щербавская Э.А. Ультразвуковая костная денситометрия в диагностике остеопенического синдрома / Э.А. Щербавская, Е.А. Кочеткова, Б.И. Гельцер // Эхография. — 2001. — Т. 2, № 4. — С. 423-427.
23. Calcium accretion in girls and boys during puberty: a longitudinal analysis / D.A. Bailley, A.D. Martin, H.A. McKay, S. Whiting et al. // J. Bone Miner Res. — 2000. — № 15. — P. 2245-2250.
24. Gadelha M.R. Efficacy of medical treatment in Cushing’s disease: a systematic review / M.R. Gadelha, L. Vieira Neto // Clinical Endocrinology. — 2014. — V. 80, № 1. — P. 1-12. — doi: 10.1111/cen.12345
25. Gluer С.С. Роль количественной ультразвуковой денситометрии в диагностике остеопороза / С.С. Gluer // Остеопороз и остеопатии. — 1999. — № 3. — С. 33-39.
26. Lukert B.P. Glucocorticoid-induced osteoporosis: pathogenesis and management / B.P. Lukert, L.G. Raisz // Ann. Intern. Med. — 1990. — V. 112(5). — P. 353-364.
27. Management of endocrine disease: The burden of Cushing’s disease: clinical and health-related quality of life aspects / R.A. Feelders, S.J. Pulgar, A. Kempel, A.M. Pereira // European Journal of Endocrinology. — 2012. — V. 167, № 3. — P. 311-326. — doi: 10.1530/ eje‑11-1095.
28. McKeage K. Pasireotide: A Review of Its Use in Cushing’s Disease / K. McKeage // Drugs. — 2013. — V. 73(6). — P. 563-574. — doi: 10.1007/s40265-013-0052-0.
29. Morgan F.H. Medical management of Cushing’s syndrome / F.H. Morgan, M. Laufgraben // Expert Review of Endocrinology & Metabolism. — 2013. — V. 8(2). — P. 183-193. — doi: 10.1586/eem.13.3.
30. Mortality and Morbidity in Cushing’s Disease over 50 Years in Stoke-on-Trent, UK: Audit and Meta-Analysis of Literature / R.N. Clayton, D. Raskauskiene, R.C. Reulen, P.W. Jones // The Journal of Clinical Endocrinology & Metabolism. — 2011. — V. 96, № 3. — P. 632-642. — doi: 10.1210/jc.2010-1942.
31. Mortality in Patients Treated for Cushing’s Disease Is Increased, Compared with Patients Treated for Nonfunctioning Pituitary Macroadenoma / O.M. Dekkers, N.R. Biermasz, A.M. Pereira et al. // The Journal of Clinical Endocrinology & Metabolism. — 2007. — V. 92, № 3. — P. 976-981. — doi: 10.1210/jc.2006-2112.
32. Multisystem Morbidity and Mortality in Cushing’s Syndrome: A Cohort Study / O.M. Dekkers, E. Horváth-Puhó, O.L. Jørgensen et al. // The Journal of Clinical Endocrinology & Metabolism. — 2013. — V. 98, № 6. — P. 2277-2284. — doi: 10.1210/jc.2012-3582
33. The European Registry on Cushing's syndrome: 2-year experience. Baseline demographic and clinical characteristics / E. Valassi, A. Santos, M. Yaneva et al. // European Journal of Endocrinology. — 2011. — V. 165(3). — P. 383-392. — doi: 10.1530/eje‑11-0272.
1. Automated electrochemicoluminescence method for the determination of cortisol in saliva for the diagnosis of endogenous hypercorticism in patients with obesity / Zh.E.Belaya, A.V.Y`l`y`n, G.A.Mel`ny`chenko [y` dr.] // Ozhy`reny`e y` metaboly`zm. - 2011. - N2. - S. 56-63. doi: 10.14341/2071-8713-4954
2. Actual problems of osteoporosis / Pod red. V.Y`.Strukova. - Ty`pografy`ya «Rostra», 2009. - S. 342.
3. Buxman A.Y`. Basic principles of X–ray and X–ray differential diagnosis of osteoporosis /A.Y`. Buxman // Mezhdunarodnыj medy`cy`nsky`j zhurnal. - 1999. - T. 2, N 3-4. - S. 213-217.
4. Vlasova Y`.S. Modern methods of radiation diagnosis of osteoporosis / Y`.S. Vlasova // Vestny`k rentgenology`y` y` rady`ology`y`. - 2002. - N 1. - S. 37-42.
5. Age features of changes in biochemical markers of bone remodeling in children / A.A.Baranov, L.A.Shheplyagy`na, M.Y`. Bakanov [y` dr.] // Ros. pedy`atr. zh. - 2002. - N 3. - S. 7-12.
6. Dedov Y`.Y`. Cushing's disease: clinical features, diagnosis, treatment / Pod redakcy`ej Y`.Y`.Dedova, G.A.Mel`ny`chenko. Prakty`cheskoe rukovodstvo dlya vrachej. – M. 2012. – S. 12-14.
7. Dedov Y`.Y`. Endocrinology: National leadership / Y`.Y`.Dedov, G.A. Mel`ny`chenko (red.). - M.: Gэotar-Medy`a; 2009. – S. 95-97.
8. Ermakova Y`.P. Serum biochemical markers in the diagnosis of osteoporosis / Y`.P.Ermakova, Y`.A. Pronchenko // Osteoporoz y` osteopaty`y`. - 1998. - N 1. - S. 24-26.
9. Kudryavcev P.S. Methods and apparatus for ultrasonic densitometry / P.S.Kudryavcev // Osteoporoz y` osteopaty`y`. - 1999. - N 2. - S. 44-47.
10. Metabolic complications of endogenous hypercorticism. Selection of patients for screening / Zh.E.Belaya, L.Ya.Rozhy`nskaya, N.V.Dragunova [y` dr.] // Ozhy`reny`e y` metaboly`zm. - 2013. - N1. - S. 26-31. doi: 10.14341/2071-8713-5068
11. Osteopenia in children: diagnosis, prevention and correction: A Handbook for doctors / L.A. Shheplyagy`na, T.Yu. Moy`seeva, M.V. Kovalenko [y` dr.]. - M., 2005. - 23 s.
12. Osteoporosis: epidemiology, clinical features, diagnosis, prevention and treatment / AMN Ukray`nы; pod red. N.A. Korzha, V.V. Povoroznyuka, N.V. Dedux, Y`.A Zupancza. - X.: Zolotыe strany`czы, 2002. - 648 s.
13. Povoroznyuk V.V. Diseases of the musculoskeletal system in people of all ages (selected lectures, reviews, articles) / V.V.Povoroznyuk: T.2 - K., 2004.- 480 s.
14. Povoroznyuk V.V. Structural and functional status of bone in children and adolescents of Ukraine: ultrasound densitometry data / V.V. Povoroznyuk // PAG. - 1999. - N 4. - S. 154.
15. Raxmanov A.S. Bone densitometry in the diagnosis of osteopenia / A.S.Raxmanov, A.V. Bakuly`n // Osteoporoz y` osteopaty`y`. - 1998. - N 1. - S. 43-45.
16. Rozhy`nskaya L.Ya. The mineral density of the tissue in endogenous and exogenous hypercorticism / L.Ya. Rozhy`nskaya // Osteoporoz y` osteopaty`y`. - 2000, N 2. - S.12-17.
17. Smiyan I.S. Secondary osteoporosis in childhood and the first experience of using of dual energy densitometry in Ukraine for its diagnosis / I.S. Smiyan // PAG. - 1999. - N 4. - S. 154.
18. The modern view on the screening and diagnosis of endogenous hypercorticism / Zh.E.Belaya, L.Ya.Rozhy`nskaya, G.A.Mel`ny`chenko, Y`.Y`. Dedov // Problemы эndokry`nology`y`. - 2012. - T. 58. - N4. - S. 35-41. doi: 10.14341/probl201258435-41.
19. Status of bone in children and adolescents according to the single–photon densitometry / N.V.Dedux, N.S.Shevchenko, S.D. Shevchenko [y` dr.] // Ortopedy`ya, travmatology`ya y` protezy`rovany`e. - 1999. - N 1. - S. 13-16.
20. Frolova T.V. Evaluation of structural and functional state of bone in school–age children and adolescents on the results of ultrasound densitometry: Method. Recommendations / T.V.Frolova, M.O.Korzh, S.P.Shklyar - Xarkiv, 2006. - 26 s.
21. Czvetnaya Y`.N. Age features of concentration of C–terminal peptides in body blood plasma in children of 1-6 years old / Y`.N.Czvetnaya, N.P. Ershova // Poly`kly`ny`ka. - N1. - 2006. - S. 52-55.
22. Shherbavskaya Э.A. Ultrasonic bone densitometry in the diagnosis of osteopenia syndrome / Э.A.Shherbavskaya, E.A.Kochetkova, B.Y`.Gel`cer // Эxografy`ya. - 2001. - T. 2, N 4. - S. 423-427.
23. Calcium accretion in girls and boys during puberty: a longitudinal analysis / D.A.Bailley, A.D.Martin, H.A.McKay, S.Whiting [et al.] // J. Bone Miner Res. – 2000. – №15. – P. 2245-2250.
24. Gadelha M.R. Efficacy of medical treatment in Cushing's disease: a systematic review / M.R. Gadelha, L.Vieira Neto // Clinical Endocrinology. – 2014. – V.80, N1. – P.1-12. doi: 10.1111/cen.12345
25. Gluer С.С. Роль количественной ультразвуковой денситометрии в диагностике остеопороза / С.С.Gluer // Остеопороз и остеопатии. – 1999. – №3. – С.33-39.
26. Lukert B.P. Glucocorticoid-induced osteoporosis: pathogenesis and management. / B.P.Lukert, L.G.Raisz // Ann. Intern. Med. – 1990. – V.112(5). – P. 353-364.
27. Management of endocrine disease: The burden of Cushing’s disease: clinical and health-related quality of life aspects / R.A.Feelders, S.J.Pulgar, A.Kempel, A.M.Pereira // European Journal of Endocrinology. – 2012. – V.167, N3. – P.311-326. doi: 10.1530/ eje-11-1095.
28. McKeage K. Pasireotide: A Review of Its Use in Cushing's Disease / K.McKeage // Drugs. – 2013. – V.73(6). – P.563-574. doi: 10.1007/s40265-013-0052-0
29. Morgan F.H., Medical management of Cushing's syndrome / F.H.Morgan, M.Laufgraben // Expert Review of Endocrinology & Metabolism. – 2013. – V.8(2). – P.183-193. doi: 10.1586/eem.13.3
30. Mortality and Morbidity in Cushing's Disease over 50 Years in Stoke-on-Trent, UK: Audit and Meta-Analysis of Literature / R.N.Clayton, D.Raskauskiene, R.C.Reulen, P.W.Jones // The Journal of Clinical Endocrinology & Metabolism. – 2011. – V.96, N3. – P.632-642. doi: 10.1210/jc.2010-1942
31. Mortality in Patients Treated for Cushing's Disease Is Increased, Compared with Patients Treated for Nonfunctioning Pituitary Macroadenoma / O.M. Dekkers, N.R.Biermasz, A.M. Pereira [et al] // The Journal of Clinical Endocrinology & Metabolism. – 2007. – V.92, N3. – P.976-981. doi: 10.1210/jc.2006-2112
32. Multisystem Morbidity and Mortality in Cushing's Syndrome: A Cohort Study / O.M.Dekkers, E.Horváth-Puhó, O.L.Jørgensen [et al.] // The Journal of Clinical Endocrinology & Metabolism. – 2013. – V.98, N6, – P.2277-2284. doi: 10.1210/jc.2012-3582
33. The European Registry on Cushing's syndrome: 2-year experience. Baseline demographic and clinical characteristics / E.Valassi, A.Santos, M.Yaneva [et al.]// European Journal of Endocrinology. – 2011. – V.165(3). – P.383-392. doi: 10.1530/eje-11-0272