Журнал «Здоровье ребенка» 6 (57) 2014
Вернуться к номеру
Risk Factor for H.Pylori Infection in Children
Авторы: Abaturov A.E., Gerasymenko O.N. - State Institution «Dnipropetrovsk Medical Academy of the Ministry of Healthcare of Ukraine», Department of Faculty Pediatrics and Medical Genetics, Dnipropetrovsk, Ukraine
Рубрики: Гастроэнтерология, Педиатрия/Неонатология
Разделы: Клинические исследования
Версия для печати
Background. The aim of this study was determine the prognostic value of medical, biological and socio-hygienic factors in the formation of H.pylori infection in children.
Methods. 283 children aged 7 to 17 years with chronic gastroduodenal pathology in the acute stage were observed. Patients were divided into two groups depending on the presence of H.pylori. The main group included 224 (79.1 %) patients with H.pylori-positive status, control group included 59 (20.9 %) patients who had H.pylori-negative status.
Results. Тhe article presents the basic medical and biological and socio-hygienic risk factors in the formation of H. pylori infection in children. With the help of mathematical program processed 145 parameters, including biomedical, social and health indicators of child development in the prenatal and postnatal periods, the clinical manifestations of chronic gastroduodenal pathology, which allowed identifying the main bio-medical and socio-hygienic risk factors of high significance (relative risk > 2.0). We have found out an association of genetic risk factors in the development of H.pylori infection in children in accordance with polymorphisms ASP299GLY of gene Toll-like receptor 4. We have determined the basic clinical and endoscopic features of chronic gastroduodenal pathology in children with H.pylori-positive status and their informational value.
Целью данного исследования было определить прогностическое значение медико-биологических и социально-гигиенических факторов в развитии инфекции H.pylori у детей.
Методы. Под наблюдением находились 283 ребенка в возрасте от 7 до 17 лет с хронической гастродуоденальной патологией в стадии обострения. Пациенты были разделены на две группы в зависимости от наличия H.pylori. Основную группу составили 224 (79,1 %) пациента с H.pylori-позитивным статусом, в контрольную группу вошли 59 (20,9 %) пациентов, которые не имели H.pylori.
Результаты. Выявлены основные медико-биологические и социально-гигиенические факторы риска развития хеликобактерной инфекции у детей. С помощью математической программы обработано 145 параметров, в том числе биомедицинские, медико-социальные показатели развития ребенка в дородовом и послеродовом периодах, клинические проявления хронической гастродуоденальной патологии, что позволило идентифицировать основные медико-биологические и социально-гигиенические факторы риска высокой значимости (относительный риск > 2,0). Обнаружена зависимость генетических факторов риска развития инфекции H.pylori у детей от варианта полиморфизма Asp299Gly гена Toll-подобного рецептора 4 (TLR4). Определены основные клинические и эндоскопические особенности хронической гастродуоденальной патологии у H.pylori-позитивных детей и их информационная значимость.
Метою цього дослідження було визначення прогностичного значення медико-біологічних і соціально-гігієнічних факторів у розвитку інфекції H.pylori в дітей.
Методи. Під спостереженням знаходилися 283 дитини у віці від 7 до 17 років з хронічною гастродуоденальною патологією в стадії загострення. Пацієнти були розділені на дві групи залежно від наявності H.pylori. Основну групу становили 224 (79,1 %) пацієнти з H.pylori-позитивним статусом, у контрольну групу увійшли 59 (20,9 %) пацієнтів, які не мали H.pylori.
Результати. Виявлено основні медико-біологічні та соціально-гігієнічні фактори ризику розвитку хелікобактерної інфекції в дітей. За допомогою математичної програми оброблено 145 параметрів, в тому числі біомедичні, медико-соціальні показники розвитку дитини в допологовому і післяпологовому періодах, клінічні прояви хронічної гастродуоденальної патології, що дозволило ідентифікувати основні медико-біологічні та соціально-гігієнічні фактори ризику високої значущості (відносний ризик > 2,0). Виявлено залежність генетичних факторів ризику розвитку інфекції H.pylori в дітей від варіанта поліморфізму Asp299Gly гена Toll-подібного рецептора 4 (TLR4). Визначено основні клінічні та ендоскопічні особливості хронічної гастродуоденальної патології в H.pylori-позитивних дітей та їх інформаційна значущість.
helicobacter pylori infection, children, risk factors, polymorphism Asp299Gly of gene TLR4.
хеликобактерная инфекция, дети, факторы риска, полиморфизм Asp299Gly гена TLR4.
хелікобактерна інфекція, діти, фактори ризику, поліморфізм Asp299Gly гена TLR4.
Статья опубликована на с. 15-19
Introduction
Helicobacter pylori (H.pylori) is conceded as the causative agent of one of the most common chronic bacterial infections of human worldwide. It is proved that at the present time about half of the world’s population is infected by H.pylori, at the same time, the prevalence of H.pylori is different in different countries. The high prevalence of H.pylori is almost always correlated with low socio-economic status of the population [4, 7]. There were no large epidemiological studies examining the infection of the population of Ukraine by H.pylori carried out.
H.pylori infection causes an inflammatory response almost at all infected individuals, but the severity of inflammation depends on the interaction of many factors, first of all, such as the virulence of the bacteria, bio-medical and socio-hygienic factors of an infected person’s organism, which predetermine the formation of H.pylori infection in children [2, 6].
Disclosure of the molecular mechanisms of non-specific innate immune defense, in particular the role of Toll-like receptors (TLR), let to clarify the meaning of the TLR in the development of H.pylori infection in children. TLR4 plays a special role in the development of infection inflammation process caused by H.pylori [1, 5].
The differences in the genes that control the body’s protective response, especially in gene regulatory molecules, providing the first stages of an inflammatory reaction, determine the nature of the inflammatory response and the flow specific immunological reactions in the development of H.pylori infection. The most common cause of differences in the structure of genes are point mutations — single nucleotide substitution, or single nucleotide polymorphism (SNP).
Of particular interest are the data on the effect of gene polymorphism responsible for the recognition H.pylori and start signal paths in the initial stages of inflammation, the character of the current child protective reactions and susceptibility to a number of diseases. Largely due to the variability of this gene polymorphism, determining elements of the innate and adaptive immunity, which includes, inter alia, transmembrane signaling TLR4. Of the 29 different gene SNP TLR4, providing detection of lipopolysaccharide (LPS) H.pylori, primarily, SNPAsp299Gly function associated with a change response to LPS H.pylori. AG mutation at position 896 of a gene encoding TLR4, leads to the substitution of asparagine by glycine at amino acid position 299 (Asp299Gly), changing the structure of the extracellular domain of TLR4 [5, 8].
The aim of this study was determine the prognostic value of medical, biological and socio-hygienic factors in the formation of H.pylori infection in children with chronic gastroduodenal pathology.
Materials and Methods
Study Population
We observed 283 children aged 7 to 17 years with chronic gastroduodenal pathology in the acute stage, who were examined and treated at a specialized children’s gastroenterology department of Public Institution «Dnipropetrovsk City Children’s Clinical Hospital № 1» of Dnipropetrovsk regional council». Patients depending on the presence of H.pylori were divided into two groups. The main group included 224 (79.1 %) patients with H.pylori-positive status. A control group included 59 (20.9 %) patients who weren’t detected H.pylori during a breath test and study for the presence of specific immunoglobulin’s (H.pylori-negative status).
Clinical and Laboratory Evaluations
Used to verify the diagnosis of clinical and medical history, endoscopy of the esophagus, stomach and duodenum was conducted for all children according to the standard technique of biopsy of the gastric mucosa (GM). For identification of H.pylori infection using rapid urease Help test and breathing Helik test (LLC AMA, Russia, St. Petersburg), the determination of venous blood serum total immunoglobulin (IgM, IgA, IgG) to Ag CagA protein H.pylori ELISA (Vector-Best, Russia).
The level of TLR4 gene expression in the GM in real time and the definition of polymorphism Asp299Gly TLR4 gene in peripheral venous blood were performed by polymerase chain reaction (PCR) in the Research Institute for Genetics and Immunological Grounds of Pathology and Pharmacogenomics (Poltava, Ukraine).
Genomic DNA was isolated using the kit for the DNA/RNA from serum or plasma (LitTeh, Russia). Gene polymorphism Asp299Gly TLR 4 was amplified by PCR in 25 l of reaction mixture containing 2.5 l of 10 x Buf amplification, 2 mM magnesium chloride, 0.2 mM of each dNTP; from 66 ng primer Asp299Gly:
F: 5’-GATTAGCATACTTAGACTACTACCTCCATG-3‘
R: 5’-GATCAACTTCTGAAAAAGCATTCCCAC-3‘
2.5 units. DNA Polymerase Tag; 20–50 ng of genomic DNA
Statistical Analysis
Statistical analysis of the results was carried out using statistical software packages Statgraf, Matstat, Statistica 6.0. With the help of mathematical program processed 145 parameters, including biomedical, social and health indicators of child development in the prenatal and postnatal periods, clinical and medical history manifestations of chronic gastroduodenal pathology and results of laboratory and instrumental investigations. Wald’s sequential analysis was used to determine the prognostic value of selected risk factors that determine the risk of H.pylori infection in children. In the study of the statistical significance of the differences of samples used parametric and non-parametric tests. The criterion of the RR was determined by the formula: RR = fb (1-Fl)/FK (1-fb), where fb — frequency of findings in patients with H.pylori-positive status, f — frequency of the trait in patients with H.pylori-negative status. Significant differences were assessed using the Student t-test for data with a normal distribution, the distribution that is different from the normal, using a non-parametric U Mann-Whitney test. For comparison, the frequency characteristic between the groups using the criterion x2 (Chi-square test) with degrees of freedom equals to 1. Evaluation of the effect of frequency variants Asp299Gly polymorphism genotype TLR4 gene was performed by calculating the epidemiological indicators — the odds ratio (OR) with the definition of the 95% confidence interval (CI). A significance level of p < 0.05 was used for all analyses [3].
Ethics Statement
The study was conducted in accordance with the ethical principles for medical research involving human subjects, adopted the Declaration of Helsinki and Good Clinical Practice. To participate in a research study, this was carried out with the permission of the local committee on bioethics, written informed consent of the parents of patients.
Results and Discussion
To assess the impact of biomedical and social-hygienic factors on the development of H.pylori infection in children was calculated relative risk (RR), diagnostic coefficient of each of the 145 studied parameters that allowed the use of dedicated most informative parameters for creating tables of probability forecast H.pylori infection in children.
The Age and Sex of the Child
There were no significant differences by gender in the study and control group were observed. Boys predominated in the group with H.pylori-positive status in contrast to the comparison group (59.38 and 55.93 %, respectively), girls — in the group of children with H.pylori-negative status (44.06 and 40.63 %), but these differences were not statistically significant (P > 0.05).
The average age of the study group patients was 13.49 ± 0.54 years, the comparison group — 13.42 ± 0.53 years (P > 0.05). At the same time, a marked increase in the risk of infection with CagA(+) strains of H.pylori and the development of H.pylori infection at the age of 12–14 years (RR = 3.25). Children with H.pylori-positive status had a higher body mass index, in contrast to the comparison group (20.54 ± 0.70 and 18.41 ± 0,56; Pu < 0.01), but the risk of H.pylori infection is no effect.
Genetic Predisposition
Family history for peptic ulcer disease, chronic gastroduodenitis, especially on the mother, the children increased the risk of the formation of H.pylori infection (RR = 2.63 and RR = 2.15, respectively).
Risk Factors for the Presence of Gene Polymorphisms Asp299Gly TLR4
The results of our molecular genetic studies have allowed to define what «wild» genotype Asp/Asp gene TLR4 was recorded with almost equal frequency in children with chronic gastroduodenal pathology under observation (in 83.87 % of patients), and at healthy individuals (96.85 %). Heterozygous variant SNP Asp/Gly TLR4 gene was detected in 16.13 % of patients under observation, indicating a high risk of having this gene variant SNP TLR4 in children with chronic inflammatory gastroduodenal diseases (OR = 8.85, P = 0.01). Among the children under observation, patients with homozygous genotype for Gly alleles were found, which is consistent with other authors [9], who also noted the low frequency of the genotype Gly/Gly in children with chronic gastritis (0.6–1.6 %), and in children with the presence of duodenal ulcers this SNP variant gene TLR4 does not stand out in any of the patients. Did homozygous SNP Gly/Gly gene TLR4 may be considered as one of factors of resistance to the development of chronic inflammation of the stomach.
We analyzed the distribution of variants of the SNP Asp299Gly gene TLR4 in children depending on H.pylori status. Thus, in a group of children with a positive H.pylori status proportion of heterozygous genotype Asp/Gly was higher than in patients with H.pylori-negative status (17.4 and 12.5 %, respectively, OR = 1.48, 95% CI 1.15–1.89; P = 0.75), showing a trend to increased risk of infection with H.pylori in children with heterozygous genotype Asp/Gly.
In patients with heterozygous variant SNP Asp299Gly gene TLR4 were some features of prognostic risk factors of H.pylori infection. So, if you have a heterozygous variant SNP Asp299Gly gene TLR4 (genotype Asp/Gly) in boys 15.80 ± 0.58 years with a body mass index in the range 13.1–18.5 increased risk of developing H.pylori infection. (RR = 1.22; RR = 1.67, respectively).
The important biological factors that contribute to the formation of H.pylori infection in children with heterozygous genotype Asp/Gly, were family history of chronic diseases of digestive tract from both parents (RR = 6.50), presence of an allergic reaction to the medication (RR = 3.17).
In children with heterozygous variant SNP Asp299Gly gene TLR4 (genotype Asp/Gly), all of whom had frequent respiratory infections, chronic tonsillitis, been ill with scarlet fever, determined by high relative risk of H.pylori infection (2.60; 3.47; 6.50, respectively).
Some influence on the risk of the formation of H.pylori infection in children with a mutant variant SNP Asp299Gly gene TLR4 had a father’s age (19.0–26.0 years, RR = 2.75), and the mother at the time of birth (33.0-40.0 years, RR = 1.56). Among patients with genotype Asp/Gly, whose parents had significant difference in age (8 years), the relative risk of infection with H.pylori dramatically increased (RR = 5.0).
Perinatal History
Pregnancy and childbirth in mothers of patients often proceeded without pathology in both groups, but the risk of the formation of H.pylori infection in children increased in the presence of the mother during pregnancy, preeclampsia I half, the threat of termination, and preterm delivery (RR = 2.55), previous abortion (RR = 2.05). Higher relative risk of H.pylori infection was observed in children born preterm (RR = 5.62), with a body weight less than 3000 g (RR = 1.51).
Effect of feeding in infancy patients at risk of deve–loping H.pylori infection at school age were mixed, with early transfer of children to artificial feeding relative risk of H.pylori infection was 2.81. At the same time, long-term, more than two years, breastfeeding rates significantly increased relative risk of H.pylori infection (RR = 3.15).
Allergic History
The first place in frequency of occurrence in the structure of allergic reactions in children with H.pylori-positive status took a food allergy, which share of 23.7 %. Allergic reactions to allergens of plant origin were detected in 8.0 % of children in the main group and in 3.4 % of patients in the comparison. However, the presence of symptoms of allergic reactions to allergens of plant origin in patients in early childhood was associated with a higher risk of formation of their H.pylori infection in school age (OR = 2.36).
Comorbidities
In children with H.pylori-positive status was a high incidence of chronic giardiasis — 52.6 % (in the group with H.pylori-negative status — 13.6 %). Development of H.pylori infection in children was associated with the presence of chronic giardiasis, the relative risk was high and amounted to 4.47.
The risk of H.pylori infection was higher in children, all of whom had earlier carried operative interventions (RR = 5.67), presence of chronic tonsillitis (RR = 3.64), autonomic dysfunction, combined with high neuroticism (RR = 3.58), the exchange dysmetabolic nephropathy (RR = 3.54), thyroid disease (RR = 3.07), frequent respiratory infections (RR = 1.71), incorrect posture (RR = 1.16).
Social and Hygiene Factors
Family Structure
Family shaping not only the identity of the child, but also provides a level of sanitary culture, the state of his health, including resistance to infectious agents. Single-parent family is one of the most common forms of family problems. Given that the child acquires H.pylori in early childhood, usually after the first year of life, and the most likely transmission of infection from mother to child and from child to child, the risk of acquiring H.pylori is highly correlated with the infectious status of the mother and brothers/sisters, and is also associated with the living conditions in overcrowded homes. For example, in a large family risk of developing H.pylori infection was 1.53 and the level of RR increased if child birth was preceded by the artificial termination of pregnancy (RR = 2.05).
Age of Parents, Education Level, Professional Employment
Some influences on the risk of the formation of H.pylori infection in children were age, education and employment of parents. Thus, the age of mothers at the birth of children less than 25 years was associated with an increase in the relative risk of infection with H.pylori (RR = 1.73). The level of education and occupation of parents ambiguous predetermined risk of H.pylori infection. Sufficiently high relative risk of formation of H.pylori infection in children were in families whose mothers have secondary and vocational (RR = 3.85), and the fathers — higher education (RR = 2.32). Professional occupation of parents was more often associated with work in the field of small business (RR = 1.29).
Material Living Conditions of the Family
Significant socio-sanitary risk factors of infection and the formation of H.pylori infection has been the lack of a centralized water supply and sanitation (RR = 2.32), the use of unboiled drinking water and accommodation in the private sector (RR = 2.05). The relative risk of the formation of H.pylori infection was 1.48 in the presence of 2.0–4.6 m2 of living space per person, and the improvement of living conditions and increase the living space and 8.0–10.0 m2 significantly reduced the level of relative risk (RR = 0.60).
By analyzing the social and hygienic factors influencing the formation of H.pylori infection in children should emphasize the importance of health education and awareness for the prevention of sanitary culture of H.pylori infection in families of children whose parents suffer from inflammatory and destructive ulcerative gastroduodenal diseases. A.P. Volosovets et al. [9] studied the effect of H.pylori therapy, H.pylori-infected parents in the level of re-infection in children with H.pylori eradication achieved, showed that the rate of reinfection among children with H.pylori eradication achieved that after treatment lived with H.pylori-uninfected parents, and was lower as compared to the children who live with H.pylori-positive parents. In connection with what is reasonable need to verify H.pylori status parents of children with chronic H.pylori-associated gastroduodenal diseases, and, if confirmed, to carry H.pylori eradication therapy H.pylori-infected parents with a child at the same time to prevent reinfection it.
The Clinical Features of Chronic Gastroduodenal Pathology in Children with H.pylori-Positive Status
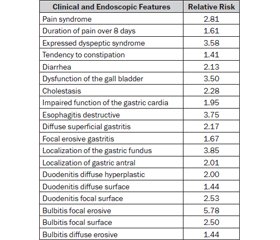
The severity and characteristics of the clinical symptoms and syndromes are different in patients with H.pylori-positive and H.pylori-negative status. The main clinical and endoscopic features of chronic gastroduodenal pathology in children with H.pylori-positive status, and the value of their information are shown in Table 1.
/18/18.jpg)
Thus, children with H.pylori-positive status were recorded more severe pain (RR = 2.81) and dyspeptic (RR = 3.58) syndromes, the presence of gall bladder dysfunction (RR = 3.50), and the inclination to cholestasis (2.28), destructive esophagitis (OR = 3.75), diffuse superficial gastritis (RR = 2.17), erosive (RR = 5.78) and the focal surface (RR = 2.50) bulbitis, diffuse hyperplastic duodenitis (RR = 2.0).
Given the high rate of clinical and diagnostic endoscopic manifestations of H.pylori infection in children with chronic gastroduodenal pathology, in our opinion, it is necessary for children with severe and prolonged pain, dyspeptic syndrome to determine H.pylori status. In the case of doubtful results in the identification of H.pylori or the lack of opportunity for laboratory confirmation of these patients having H.pylori, eradication should be carried H.pylori therapy, based on clinical and/or endoscopic data.
Conclusions
1. With the help of mathematical program processed 145 parameters, including biomedical, social and health indicators of child development in the prenatal and postnatal periods, the clinical manifestations of chronic gastroduodenal pathology, which allowed identifying the main bio-medical and socio-hygienic risk factors of high significance (RR > 2.0)
2. Depending on the polymorphism Asp299Gly gene TLR4 (genotype Asp/Gly) highlights the most significant risk factors for H.pylori infection in children: the presence of family history of chronic diseases of the digestive tract of both parents, been ill with scarlet fever, the presence of chronic tonsillitis, allergic reactions to drugs, tendency to frequent respiratory infections.
3. The main features of the clinical manifestations of chronic gastro-duodenal pathology in children with H.pylori-positive status, having a high informational value, include: the severity and duration of pain, dyspeptic syndromes, the presence of gall bladder dysfunction, addiction to cholestasis, destructive esophagitis, and diffuse superficial gastritis, erosive and the focal surface bulbitis, diffuse hyperplastic duodenitis.
Competing Interests
All authors declare that they have no conflict of interest.
1. Abaturov A.E., Volosovets A.P., Yulish E.I. The initiation of the inflammatory process in viral and bacterial diseases, opportunities and prospects for drug control [In Russian]. — Kharkov: LLC S.A.M., 2011. — 392.
2. Amieva M.R., El-Omar E. Host bacterial interaction in Helicobacter pylori infection // Gastroenterology. — 2008. — 134 (1). — 306-32; doi:10.1053/j.gastro.2007.11.009.
3. Antomonov M.Ju. Mathematical processing and analysis of biomedical data [In Russian]. — K.: Fіrma malogo druku, 2006. — 558.
4. Consequences of Helicobacter pylori infection in children / L. Pacifico, C. Anania, J.F. Osborn, F. Ferraro, C. Chiesa // World J. Gastroenterol. — 2010, Nov 7. — 16(41). — 5181-5194; doi: 10.3748/wjg.v16.i41.5181.
5. Expression TLR4 and TLR-accessory molecules in children with chronic gastroduodenitis [In Ukrainian] / A.Е. Abaturov, O.N. Gerasymenko, O.A. Shlykova, I.P. Kaidashev // Child’s Health. — 2013. — 6 (49). — 14-18.
6. Helicobacter pylori infection is strongly associated with gastric and duodenal ulcers in a large prospective study / B. Schöttker, M.A. Adamu, M.N. Weck [et al.] // Clin. Gastroenterol. Hepatol. — 2012 May. — 10(5). — 487-93.e1; doi: 10.1016/j.cgh.2011.12.036. Epub 2012 Jan 8.
7. Pilot study: miscellaneous therapy is highly successful for Helicobacter pylori eradication / F. Sierra, J.D. Forero, M. Rey [et al.] // Aliment. Pharmacol. Ther. — 2013 Jun. — 37(12). — 1165-71; doi: 10.1111/apt.12329. Epub 2013 May 8.
8. Toll-like receptor (TLR2, TLR4 and TLR5) gene polymorphisms and Helicobacter pylori infection in children with and without duodenal ulcer / S.B. Moura, L.R. Almeida, J.B. Guerra [et al.] // Microbes Infect. — 2008 Nov-Dec. — 10 (14–15). — 1477-83; doi: 10.1016/j.micinf.2008.08.009. Epub 2008 Sep 4.
9. Volosovets O.P., Saltanova S.D. Effect of Helicobacter therapy H.pylori-infected parents to the level of re-infection in children H.pylori eradication achieved [In Ukrainian] // Child’s Health. — 2012. — 2 (37). — 25-27.